Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Update on Parkinson’s Disease
*Corresponding author: Jorge Garza-Ulloa, Research Consulting Services garzaulloa.org, University of Texas El Paso, USA.
Received: April 16, 2019; Published: May 03, 2019
DOI: 10.34297/AJBSR.2019.02.000614
Abstract
Parkinson’s disease (PD) is a progressive nervous system disorder that affect movement and present other symptoms, that can be different for everyone and the exact cause of this damage is still unknown. Parkinson’s disease can’t be cured, medications and surgeries might significantly improve their symptoms, these must be prescribed by the neurologist, but it is important to understand how the medication works, what do we expect from them and what other options are available today. In this review the goal is introduce and explain to PD patients and their caregivers the PD: symptoms, stages, treatments, causes and types.
Keywords: Parkinson’s disease; Tremors; Movement disorders; Postural instability; Levodopa; Parkinsonism; Idiopathic Parkinson’s; Atypical parkinsonism
Abbrevations: PD: Parkinson’s Disease; CNS: Central Nervous System; MRI: Magnetic Resonance Imaging; STN: Subthalamic Nucleus; GPI: Globus Pallidus Internal; DBS: Deep Brain Stimulation; IPG: Implanted Pulse Generator; UPDRS: Unified Parkinson’s Disease Rating Scale; L-DOPA: Levodopa; LRRK2: Leucine-Rich Repeat Kinase 2; PARK7: Parkinsonism Associated Deglycase; PRKN: Parkin Rbr E3 Ubiquitin Protein Ligase; TMS: Transcranial Magnetic Stimulation; THC: Tetrahydrocannabinol; CBD: Cannabidiol; TCE: Trichloroethylene; CSE: Chronic Solvent Encephalopathy; MSA: Multiple System Atrophy; PSP: Progressive Supranuclear Palsy; CBS: Corticobasal Syndrome; DLB: Dementia with Lewy Bodies; VP: Vascular Parkinsonism; PBA: Pseudobulbar Affect
Introduction
Parkinson’s Disease (PD) is a progressive neurodegenerative disease producing neuronal cell death, presenting loss of dopamineproduction in the brain area known as substancia nigra [1], altering the central nervous system CNS (brain and spinal cord), and affecting the regulation of the human movements and emotions. the exact cause of this damage is still unknown, and currently there is no cure for Parkinson’s disease. PD is a form of extrapyramidal disorder that affects movements disorder caused by damage to the extrapyramidal tract, a network of nerves that controls movements.
PD is a typical movement disorder [2] and the 2nd most common neurodegenerative condition after Alzheimer’s disease. PD is a continuous neurological disorder where the symptoms continue to worsen gradually [3]. PD is a highly variable disease, meaning that different patients have different combinations of symptoms, and those symptoms can be at varying severity levels.
Symptoms of PD
The main symptoms of PD are of three kinds: primary motors, secondary motors and non-motors [4]. Where
Motors (Directly Related to Movement)
a. Tremors (shaking) in the limbs,
b. Rigidity (muscle stiffness),
c. Bradykinesia (slowness of movements),
d. Postural instability (impaired balance or difficulty standing or walking,
Secondary Motor (Consequence of Movement Disorders)
a. Hypomimia - loss of facial expressions known also as Parkinson mask.
b. Freezing of gait or shuffling gait – the gait, or way of walking, may be affected by a temporary hesitation (freezing) or dragging of the feet (shuffling).
c. Unwanted accelerations – movements which are too quick, which may appear in movement or in speech.
d. Speech difficulty or changes in speech – including slurred speech or softness of voice e. Stooped posture – the body leans forward, and the head may be slightly turned down.
f. Dystonia – prolonged muscle contractions that can cause twisting of body parts or repetitive movements.
g. Impaired fine motor dexterity – difficulty with precise hand and finger movement, such as in writing, sewing, or fastening buttons.
h. Poverty of movement – lack of natural, subtle movements like the decreased arm swing during walking
i. Akathisia – restless movement, which may appear as being jumpy or fidgety.
j. Difficulty swallowing – challenges swallowing can also cause drooling or excess saliva.
k. Cramping – muscles may stay in a contracted position and cause pain
l. Sexual dysfunction – decreased sex drive, inability to orgasm, erectile dysfunction in men, decreased lubrication in women, or pain with intercourse in women.
Non-Motors (no Related to Movement Disorders)
a. Fatigue – excessive tiredness that isn’t relieved with sleep
b. Digestive issues – difficulty swallowing, nausea, bloating, and/or constipation
c. Sleep problems – including difficulty falling asleep, staying asleep, vivid dreams, physically acting out dreams, sleep apnea and sleep attacks (patients may be suddenly overcome with drowsiness and fall asleep).
d. Orthostatic hypotension – low blood pressure that occurs when rising to a standing position.
e. Increased sweating.
f. Increased drooling.
g. Pain – which may accompany muscle rigidity.
h. Hyposmia – reduced sense of smell.
i. Mood changes – including apathy, depression, anxiety and Pseudobulbar Affect PBA (frequent, involuntary and uncontrollable outbursts of crying or laughing)
j. Cognitive changes – including memory difficulties, slowed thinking, confusion, impaired visual-spatial skills (such as getting lost in familiar locations), and dementia.
k. Psychotic symptoms – including hallucinations, paranoia, and agitation.
l. Incontinence _Urinary problems.
m. Orthostatic hypotension (OH) - change of arterial pressure with postural changes
n. Melanoma - an invasive form of skin cancer that has been found to develop more often in people with Parkinson’s.
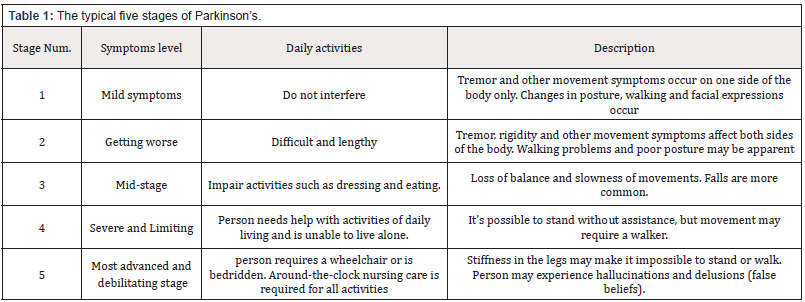
PD stages
There are typical patterns of progression in Parkinson’s disease that are defined in five stages, Not everyone will experience all the symptoms of Parkinson’s, and if they do, they won’t necessarily experience them in quite the same order or at the same intensity. The typical five stages are summarized in (Table 1).
PD Treatments
There are a variety of treatments that can help manage the motor symptoms and improve the quality of life, but there is no known treatment to stop or slow the disease progression that is different in each patient. The current treatments available must be prescribed by a neurologist, these are: medications, surgical treatments and complementary/alternative therapies.
Medications
Levodopa is the most efficacious medication for PD, it is converted to dopamine. When initiated the levodopa treatment improves symptoms through the day and night. Overtime patients develop OFF time. Off time is the time during the day when PD symptoms return or worsen, typically 40% in 5 years, 90% in 10 years [1]. Off time PD symptoms may include motor, secondary motors and non-motors. Off periods is the sum of four times that levodopa is not working:
a. Early morning Off -patients typically present with poor motor function in the morning when they wake up, before the first dose of levodopa [6],
b. Wearing Off - symptoms of Parkinson’s start to return or worsen before the next dose of levodopa is due [7],
c. Delayed On – delay in the onset of benefit of a levodopa dose [8],
d. Dose Failure - when there is no benefit from dose of levodopa [9].
Current medication for PD [10].
Levodopa - The most potent medication for Parkinson’s disease (PD) is levodopa. Its development in the late 1960s represents one of the most important breakthroughs in the history of medicine. Levodopa in pill form is absorbed in the blood from the small intestine and travels through the blood to the brain, where it is converted into dopamine, needed by the body for movement. Plain levodopa produces nausea and vomiting.
a. Carbidopa/levodopa remains the most effective drug to treat PD. The addition of carbidopa prevents levodopa from being converted into dopamine prematurely in the bloodstream, allowing more of it to get to the brain. Therefore, a smaller dose of levodopa is needed to treat symptoms [11].
b. Carbidopa/levodopa (Sinemet®)- Levodopa is combined with carbidopa to prevent nausea and vomiting as side effect.
c. Carbidopa/levodopa (Rytary®) is a combination of long and short-acting capsule.
d. Carbidopa/levodopa (Parcopa®) is formulation that dissolves in the mouth without water.
e. Carbidopa/levodopa (Stalevo®) is combined formulation that includes the COMT inhibitor entacapone.
f. Dopamine Agonists [12]. They stimulate the parts of the human brain influenced by dopamine. In effect, the brain is tricked into thinking it is receiving the dopamine it needs. Dopamine agonists can be taken alone or in combination with medications containing levodopa. The most commonly prescribe oral pill are: pramipexole (Mirapex), ropinirole (Requip), rotigotine transdermal system (Neupro®), Bromocriptine (Parlodel®) and one special apomorphine (Apokyn), is a powerful and fast-acting injectable medication that promptly relieves symptoms of PD within minutes, but only provides 30 to 60 minutes of benefit. Its main advantage is its rapid effect. It is used for people who experience sudden wearing-off spells when their PD medication abruptly stops working, leaving them unexpectedly immobile.
g. Amantadine. it is a mild agent that is used in early PD to help tremor. In recent years, amantadine has also been found useful in reducing dyskinesias that occur with dopamine medication. h. COMT Inhibitors are used to prolong the effect of levodopa by blocking its metabolism. COMT Inhibitors are used primarily to help with “wearing off,” in which the effect of levodopa becomes short-lived. The most common are: Carbidopa/ levodopa (Stalevo®), Entacapone (Comtan®) and Tolcapone (Tasmar®)
i. Anticholinergic Drugs. They decrease the activity of acetylcholine, a neurotransmitter that regulates movement. It can be helpful for tremor and may ease dystonia associated with wearing-off or peak-dose effect. The most common are: trihexyphenidyl (Artane®), benztropine mesylate (Cogentin®) and procyclidine (no longer available in the U.S.), among others.
j. MAO-B Inhibitors. They block an enzyme in the brain that breaks down levodopa, this makes more dopamine available and reduces some of the motor symptoms of PD. When used together with other medications, MAO-B inhibitors may reduce “off” time and extend “on” time. They have been shown to delay the need for Sinemet when prescribed in the earliest stage of PD and have been approved for use in later stages of PD to boost the effects of Sinemet. The most common used are: Selegiline also called Depreny (Eldepryl® and Zelapar®) and rasagiline (Azilect®).
Caution: PD medications may have interactions with certain foods, other medications, vitamins, herbal supplements, over the counter cold pills and other remedies. Anyone taking a PD medication should talk to their doctor and pharmacist about potential drug interactions.
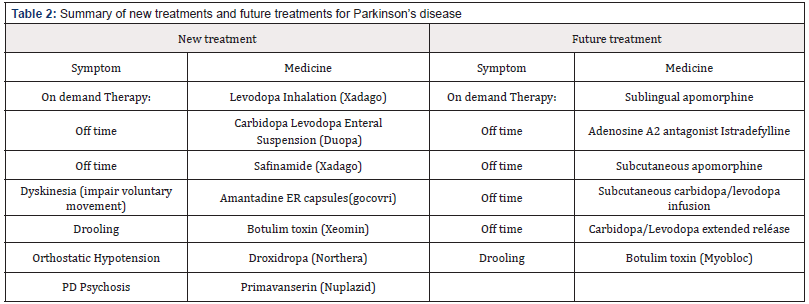
A summary of new treatments and future treatments for Parkinson’s disease are shown in (Table 2) [5]
Surgical Treatments
Surgical treatments can be an effective treatment option for different symptoms of Parkinson’s disease (PD), only the symptoms that previously improved on levodopa have the potential to improve after the surgery. Surgical treatment is reserved for PD patients who have exhausted medical treatment of PD tremor or who suffer profound motor fluctuations (wearing off and dyskinesias), surgical treatments doesn’t cure PD and it does not slow PD progression. These are:
a. Carbidopa/levodopa intestinal fusion pump (DUOPA™). This is a gel formulation of the drug that requires a surgicallyplaced tube. provides 16 continuous hours of carbidopa and levodopa for motor symptoms. The small, portable infusion pump delivers carbidopa and levodopa directly into the small intestine obtaining better ON time.
b. Deep brain stimulation DBS [13]. DBS is only recommended for people who have had PD for at least four years and have motor symptoms not adequately controlled with medication. In DBS surgery, electrodes are inserted into a targeted area of the brain, using MRI (magnetic resonance imaging) and recordings of brain cell activity during the procedure. A second procedure is performed to implant an implanted pulse generator IPG, impulse generator battery (like a pacemaker). The IPG is placed under the collarbone or in the abdomen. The IPG provides an electrical impulse to a part of the brain involved in motor function. Those who undergo DBS surgery are given a controller to turn the device on or off. The most commonly utilized brain targets include the subthalamic nucleus (STN) and the Globus pallidus internal (GPI). Target choice should be tailored to a patient’s individual needs. The STN does seem to provide more medication reduction, while GPi may be slightly safer for language and cognition. Although most people still need to take medication after undergoing DBS, many people experience considerable reduction of their PD symptoms and can greatly reduce their medications. The amount of reduction varies from person to person.
Future Surgical Treatments
PD Stem Cell Therapy. Cell transplantation in PD patients include [14-16]: adrenal medullary, retinal, carotid body, patient’s fat (adipose tissue) and human and porcine fetal cells. Cell transplantation using aborted 6 to 9 weeks-old human embryos evolved historically as the most promising approach. One of the major concerns in cell transplantation for PD is the host immune response to the grafted tissue. Cell therapy for PD have been associated with significant concerns and complications.
Although the brain is often considered “immune-privileged”, there is in fact evidence that intracerebral immunologicallymediated graft rejection can and does occur [17]. The open-label studies, and the functional engraftment of the transplanted tissue – are enough to provide hope that improvements in cell replacement strategies for PD could yield tremendous positive impact on patients’ lives. The Food and Drug Administration FDA has not yet approved stem cell therapy as a treatment for Parkinson’s disease, clinical studies have demonstrated safety and potential efficacy. The FDA, however, requires further investigation before these kinds of treatment can be approved.
Complementary/Alternative Therapies
There many common Parkinson’s alternative available therapies for PD it is recommended speak with your doctor before, embarking on an alternative therapy. The most common are [18]:
a. Acupuncture, Acupuncture is recognized as a viable treatment for various illnesses and conditions. Acupuncture may improve PD‐related fatigue, but real acupuncture offers no greater benefit than sham treatments. PD‐related fatigue should be added to the growing list of conditions that acupuncture helps primarily through nonspecific or placebo effects [19].
b. Guided imagery (guided meditation), a gentle but powerful technique that focuses the imagination in proactive, positive ways. Motor imagery is a mental process by which an individual rehearses or simulates a given action. It is widely used in sport training as mental practice of action, neurological rehabilitation, and has also been employed as a research paradigm in cognitive neuroscience and cognitive psychology to investigate the content and the structure of covert processes (i.e., unconscious) that precede the execution of action. Motor imagery is thought to be helpful in treatment of neurological motor disabilities caused by stroke, Parkinson’s disease and spinal cord injuries [20].
c. Chiropractic. The theory of chiropractic care is based on the idea that the properly adjusted body, particularly the spine, is essential for health, with influence on life force and good health attained using spinal manipulation therapy for the removal of subluxations. The dosage of chiropractic care depends on the practitioner [21]. Some reports shown that the use of alternative treatment as chiropractic procedures appeared to help in Parkinson disease signs and symptoms [22].
d. Yoga, though yoga is one of the widely used mind-body medicine for health promotion, disease prevention and as a possible treatment modality for neurological disorders. Among various types of mind-body exercises, yoga was reported to be the largest and to produce the most significant beneficial effect in reducing Unified Parkinson’s Disease Rating Scale UPDRS III scores for people with mild to moderate PD [23].
e. Hypnosis might represent an interesting complementary therapeutic approach to movement disorders, as it considers not only symptoms, but also well-being, and empowers patients to take a more active role in their treatment. Well-designed studies considering some specific methodological challenges are needed to determine the possible therapeutic utility of hypnosis in movement disorders. In addition to the potential benefits for such patients, hypnosis might also be useful for studying the neuroanatomical and functional underpinnings of normal and abnormal movements [24].
f. Biofeedback seems to be a promising tool to improve gait outcomes for both healthy individuals and patient groups. However, due to differences in study designs and outcome measurements, it remains uncertain how different forms of feedback affect gait outcomes [25].
g. Aromatherapy uses plant materials and aromatic plant oils, including essential oils, and other aroma compounds for the purpose of altering one’s mood, cognitive, psychological or physical well-being. Aromatherapy in PD improve restlessness; anxiety, mood, works great; calming; relaxation; nausea; alertness; helped sleep; calming effect [26].
h. Herbal remedies are medication prepared from plants, including most of the world’s traditional remedies for disease. There are many herbal remedies that can be useful for PD but there are missing systematic approaches to test each one in neurologic diseases like PD. For example, Resveratrol as a natural polyphenolic compound extracted from red grapes, exerts neuroprotective effects on oxidative damage and neuronal damage through its antioxidant as well as antiinflammatory properties. Resveratrol has the potential to treat PD by inhibiting neuro-inflammation, apoptosis and promoting neuronal survival and can serve as a complementary medicine drug to reduce the L-DOPA dose needed to ameliorate PD [27].
i. Magnetic therapy, many studies conclude that further studies are needed on PD magnetic therapy. Investigations using repetitive Transcranial Magnetic Stimulation TMS in assessing the motor system function are still in an early phase and need further evaluation. Altogether, the value of TMS for studies of the physiology and pathophysiology of the motor system is beyond any doubt and the limits of these techniques have not yet been reached [28].
j. Massage. Parkinson’s disease typically causes muscle stiffness and rigidity, individuals who utilize massage therapy find it helps to alleviate joint and muscle stiffness.
k. Marijuana also called cannabis, is made up of two major parts: Tetrahydrocannabinol (THC) and cannabidiol (CBD). THC is the major part that causes one to feel “high.” THC can cause hallucinations and anxiety and is therefore to be used with caution, if at all, in Parkinson disease. CBD, by comparison, may help with sleep and anxiety. A few studies have suggested that marijuana helps with some aspects of Parkinson’s and may allow a person to reduce his or her use of prescription medications. But there is no definitive data on what dose of what parts of marijuana are helpful or harmful in Parkinson’s disease. The possible association of cannabinoid receptors with ubiquitin pathway needs to be studied further in order to understand its extensive role in PD. Furthermore, epigenetic modifications resulted by cannabinoid receptor activation needs to be elucidated which can be crucial to follow up the pathology of the disease [29].
PD causes
Around 80% populations with PD are considered as idiopathic because of their unknown source of etiology whereas the remaining 20% cases are presumed to be genetic. Variations in the genetic combination of certain genes elevate the risk of PD. Studies have reported that mutation in the LRRK2 (leucine-rich repeat kinase 2),PARK7 (Parkinsonism Associated Deglycase), PRKN (Parkin RBR E3 Ubiquitin Protein Ligase), PINK1 (PTEN-induced putative kinase 1) or SNCA (alpha-synuclein) contribute to the risk of PD[30].
Factor for Parkinson’s disease
Generally, scientists speculate that the interaction between gene mutations and environmental exposures can contribute to PD progression. Studies have listed few modifiable risk factors for PD, the following factors are considered as some of the causative factors of PD [31,32] are:
Exposure to pesticide: The evidence that pesticide and herbicide use is associated with an increased risk in PD, begs the question – are there specific pesticides that are most concerning? When data is collected on this topic in large populations, often the participants in the study are unaware of which specific pesticide or herbicide exposures they have had. This makes it difficult to determine which pesticides to avoid. From that data emerged paraquat and rotenone as the two most concerning pesticides [33] and Glyphosate as herbicide [34]. Where:
a. Paraquat’s mechanism of action is the production of reactive oxygen species, intracellular molecules that cause oxidative stress and damage cells.
b. Rotenone’s mechanism of action is disruption of the mitochondria, the component of the cell that creates energy for cell survival.
c. Glyphosate is the world’s most heavily applied herbicide, and an active ingredient in Roundup®
d. Well-water drinking. Rural residents who drink water from private wells are much more likely to have Parkinson’s disease, a finding that bolsters theories that farm pesticides may be partially to blame, according to a new California study [35].
e. Heavy metals, such as iron and manganese, are involved in neurologic disease. Most often these diseases are associated with abnormal environmental exposures or abnormal accumulations of heavy metals in the body. Many epidemiological studies have shown an association between PD and exposure to metals such as: mercury, lead, manganese, copper, iron, aluminium, bismuth, thallium, and zinc [38]. The combination of high concentration of iron and the neurotransmitter, dopamine, may contribute to the selective vulnerability of the brain in the substantia nigra pars compacta (SNpc) in the basal ganglia [36].
f. Solvents, case reports of parkinsonism, including PD, have been associated with exposures to various solvents, most notably trichloroethylene (TCE) [37]. The peripheral nervous system as well as the central nervous system can both be targeted. Prolonged workplace exposure to organic solvents can induce a chronic solvent encephalopathy (CSE) that persists even after the exposure is terminated [38].
g. Calcium, the international team, led by the University of Cambridge, found that calcium can mediate the interaction between small membranous structures inside nerve endings, which are important for neuronal signaling in the brain, and alpha-synuclein, the protein associated with Parkinson’s disease. Excess levels of either calcium or alpha-synuclein may be what starts the chain reaction that leads to the death of brain cells [39]. Ca2+ dysregulation and the direct consequences for mitochondrial health in PD [40].
h. Age, Parkinson’s disease can both be early- and late-onset. Many processes affected in Parkinson’s disease are linked to factors associated with age. The risk of Parkinson’s disease increases dramatically in individuals over the age of 60 and it is estimated that more than 1% of all seniors have some form of the condition [41].
i. Gender, more men than women are diagnosed with Parkinson’s disease (PD), and several gender differences have been documented in this disorder. One possible source of malefemale differences in the clinical and cognitive characteristics of PD is the effect of estrogen on dopaminergic neurons and pathways in the brain [42]
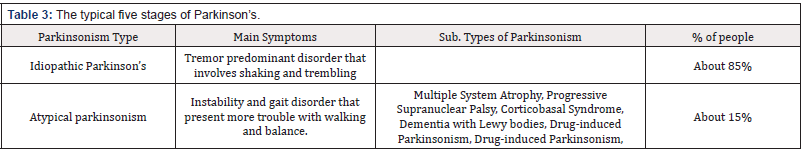
Parkinson ‘s diseases types
Parkinsonism is a constellation of signs and symptoms that are characteristically observed in Parkinson’s disease (PD), but that are not necessarily due to PD. Parkinsonism is the primary type of hypokinetic movement disorder. Parkinsonism describe the collection of signs and symptoms found in Parkinson’s disease (PD). These include slowness (bradykinesia), stiffness (rigidity), tremor and imbalance (postural instability). There are basically two general Parkinson’s types: Idiopathic Parkinson’s and atypical parkinsonism [43] (Table 3).
Idiopathic Parkinson’s
Idiopathic Parkinson’s is the most common form of Parkinsonism. It is a tremor predominant disorder that involves shaking and trembling. About 85% of people with parkinsonism have idiopathic Parkinson’s. This type of Parkinson’s disease can begin at an earlier age but progresses more slowly. It has a lower risk of cognitive (brain function) decline, but the tremors may be more difficult to treat than other symptoms [44].
Atypical parkinsonism
Atypical parkinsonism is less common, it is an instability and gait disorder that present more trouble with walking and balance. About 15% of people with parkinsonism have Atypical parkinsonism disorders, these are rarer conditions and more difficult to treat. This type of Parkinson’s disease happens at an older age but tends to progress quickly. Although people may experience fewer tremors or no tremors at all, they have a higher risk of cognitive decline. Atypical parkinsonism includes the following variations:
a. Multiple System Atrophy MSA includes several neurodegenerative disorders in which one or more systems in the body deteriorates as: incoordination (ataxia), dysfunction in the autonomic nervous system that automatically controls things such as blood pressure and bladder function. These are in addition to variable degrees of parkinsonism including symptoms such as slowness, stiffness and imbalance. Average age of onset is in the mid-50’s.
b. Progressive Supranuclear Palsy PSP is the most common degenerative type of atypical parkinsonism. Symptoms tend to progress more rapidly than PD. People with PSP may fall frequently early in the course of disease. Later symptoms include limitations in eye movements, particularly looking up and down, which also contributes to falls. Those with PSP also often have problems with swallowing (dysphagia), difficulty in producing speech (dysarthria), sleep problems, memory and thinking problems (dementia). Its average age of onset is in the mid-60’s.
c. Corticobasal Syndrome CBS is the least common of the atypical causes of Parkinsonism. Usually begins with symptoms affecting one limb. In addition to parkinsonism, other symptoms can include abnormal posturing of the affected limb (dystonia), fast, jerky movements (myoclonus), difficulty with some motor tasks despite normal muscle strength (apraxia), difficulty with language (aphasia) among others. Typically begins after age 60 [45].
d. Dementia with Lewy bodies DLB is a progressive, neurodegenerative disorder in which abnormal deposits of a protein called alpha-synuclein build up in multiple areas of the brain. It is second to Alzheimer’s as the most common cause of degenerative dementedly first causes progressive problems with memory and fluctuations in thinking, as well as hallucinations. These symptoms are joined later in the course of the disease by parkinsonism with slowness, stiffness and other symptoms like PD.
e. Drug-induced Parkinsonism is the most common form of what is known as secondary parkinsonism. Side effects of some drugs, especially those affecting brain dopamine levels (anti-psychotic or anti-depressant medication), can cause parkinsonism. Although tremor and postural instability may be less severe, this condition may be difficult to distinguish from Parkinson’s. Some medications can cause the development of Parkinsonism as: Antipsychotics, some antidepressants, reserpine, some calcium channel blockers and others. Usually after stopping those medications parkinsonism gradually disappears over weeks to months, though symptoms may last for up to a year.
f. Vascular Parkinsonism VP is based in evidences that suggest that multiple small strokes in key areas of the brain may cause Parkinsonism. A severe onset of parkinsonism immediately following (or progressively occurring within a year of) a stroke may indicate VP.
Conclusions
Parkinson’ disease is a neurologic disease that affect the functionality if the brain modifying the neural connectivity due to cell death. All medication and procedures available today only help to improve the quality of life of the patients, there is a big necessity to focus in more ways to accelerate the research on PD, like creating a cloud database with information about the development, new medications available, new surgical procedures, new way to early detection, new criteria’s and many other factors.
References
- https://www.parkinson.org/understanding-parkinsons/what-isparkinsons Accessed April 2019
- Jorge Garza Ullo (2018) Applied Biomechatronic Using Mathematical Models. Elsevier, Academic Press.
- Shreya Bhat, U Rajendra Acharya, Yuki Hagiwara, Nahid Dadmehr, Hojjat Adeli (2018) Parkinson’s disease: Cause factors, measurable indicators, and early diagnosis. Computers in Biology and Medicine 102: 234-241.
- https://parkinsonsdisease.net/symptoms/ Accessed April 2019
- https://www.parkinson.org/Understanding-Parkinsons/What-is- Parkinsons/Stages-of-Parkinsons Accessed April 2019
- Rajesh Pawha. PD Medication. What´s new Expert briefing Parkinson foundation.
- Rieko Onozawa, Jun Tsugawa, Yoshio Tsuboi, Jiro Fukae, Takayasu Mishima, et al. (2016) The impact of early morning off in Parkinson’s disease on patient quality of life and caregiver burden. Journal of the Neurological Sciences 364: 1-5.
- https://www.epda.eu.com/about-parkinsons/symptoms/motorsymptoms/ wearing-off-and-motor-fluctuations/ Accessed April 2019
- Advances in Clinical Neuroscience and Rehabilitation ACNR, http:// www.acnr.co.uk/2015/06/in-parkinsons-disease-patients-may-sufferfrom- delayed-on-as-well-as-wearing-off-which-is-more-important/ Accessed April 2019
- American Parkinson disease association APDA, http://www.aoic.net/ APDA/APDA1609arc/APDA%20Motor%20Fluctuations%20Fact%20 Sheet.pdf Accessed April 2019
- https://www.webmd.com/parkinsons-disease/guide/drugtreatments# 1 Accessed April 2019
- https://www.parkinson.org/Understanding-Parkinsons/Treatment/ Prescription-Medications/Levodopa Accessed April 2019
- https://www.parkinson.org/Understanding-Parkinsons/Treatment/ Prescription-Medications/Dopamine-Agonists Accessed April 2019
- https://www.parkinson.org/Understanding-Parkinsons/Treatment/ Surgical-Treatment-Options/Deep-Brain-Stimulation Accessed April 2019
- Lindvall (2016) Clinical translation of stem cell transplantation in Parkinson’s disease. J Intern Med 279(1): 30-40.
- Kai-C Sonntag, Bin Song, Nayeon Lee (2018) Pluripotent stem cell-based therapy for Parkinson’s disease: Current status and prospects. Progress in Neurobiology 168: 1-20.
- A Bjorklund, JH Kordower (2013) Cell therapy for Parkinson’s disease: what next? Mov Disord 28(1): 110-115.
- K C Sonntag (2007) Immunological considerations in CNS transplants Cellular Transplantation. Elsevier pp. 305-326
- https://parkinsonrockies.org/live-well/treatments-and-therapies/ other-therapies/
- John D Mark (2018) In Integrative Medicine pp. 288-299.
- Joesph Bova DC, Sergent A (2014) Chiropractic Management of an 81-Year-Old Man With Parkinson Disease Signs and Symptoms. Journal of Chiropractic Medicine 13(2): 116-20.
- J Y Kwok, K C Choi, H Y Chan (2016) Effects of mind-body exercises on the physiological and psychosocial wellbeing of individuals with Parkinson’s disease:a systematic review and meta-analysis. Complement Ther Med 29: 121-131.
- C Flamand-Roze, I Célestin-Lhopiteau, E Roze (2016) Hypnosis and movement disorders: State of the art and perspectives. Revue Neurologique 172(8-9): 530-536.
- Linda MA, van Gelder (2018) The use of biofeedback for gait retraining: A mapping review. Clinical Biomechanics 159: 159-166.
- Sarah Donley, Sadie McGregor, Wielinski C, Nance M (2019) Use and perceived effectiveness of complementary therapies in Parkinson’s disease. Parkinsonism & Related Disorders 58: 46-49.
- Qianqian Liu, Dashuai Zhu, Jiang P, Tang X , Lang Q ,et al. (2019) Resveratrol synergizes with low doses of L-DOPA to improve MPTPinduced Parkinson disease in mice. Behavioural Brain Research 367: 10-18.
- Reinhard Dengler, F Cassim (2008) The potential of transcranial magnetic stimulation (TMS) in studies of the motor function. Clinical Neurophysiology 119: 226.
- H C Dijkerman, M Ietswaart, M Johnston (2010) Motor imagery and the rehabilitation of movement disorders: an overview Neurophysiol. Found Ment Mot Imag pp. 127-144.
- Benzi M Kluger, Dylan Rakowski, Mary Christian, Daisy Cedar, OMD Ban Wong, et al. (2016) Randomized, Controlled Trial of Acupuncture for Fatigue in Parkinson’s Disease. Mov Disord 31(7): 1027-1032
- Shreya Bhat, U Rajendra Acharya, Hagiwara Y, Dadmehr N, Adeli H, et al. (2018) Parkinson’s disease: Cause factors, measurable indicators, and early diagnosis. Computers in Biology and Medicine 102: 234-241.
- C.M Tanner (2011) Environmental factors and Parkinson’s: what have we learned?
- J Campdelacreu (2014) Parkinson’s disease and Alzheimer disease: environmental risk factors. Neurologia 29(9): 541-549.
- Rebecca Gilbert (2018) The Relationship Between Pesticides and Parkinson’s.
- Mariah Caballero, Solmaz Amiri, Justin T Denney, Pablo Monsivais, Perry Hystad, et al. (2018) Glyphosate Herbicide Exposure Linked to Parkinson’s Disease. Int J Environ Res Public Health 15(12): 2885.
- Marla Cone (2009) Rural Well Water Linked to Parkinson’s Disease. Environmental Health News, Scientific America.
- Bjorklund G, Stejskal V, Urbina MA, Dadar M, Chirumbolo S, et al. (2018) Metals and Parkinson’s Disease: Mechanisms and Biochemical Processes. Curr Med Chem 25(19): 2198-2214
- Montgomery EB (1995) Heavy metals and the etiology of Parkinson’s disease and other movement disorders. Toxicology 97(1-3): 3-9.
- Edward A Lock (2012) Solvents and Parkinson disease: A systematic review of toxicological and epidemiological evidence.
- J Reis, E Benbrick, V Bonneterre, P S Spencer (2016) Parkinson’s disease and solvents: Is there a causal link? Revue Neurologique 172(12): 761- 765.
- Janin Lautenschläger, Amberley D Stephens, Fusco G, Ströhl F, Curry N, et al. (2018) C-terminal calcium binding of Alpha-synuclein modulates synaptic vesicle interaction. Nature Communications 9(1): 712.
- Marthe H R Ludtmann, Andrey Y Abramov (2018) Mitochondrial calcium imbalance in Parkinson’s disease. Neuroscience Letters 663: 86-90.
- Rashed Abdullah, Indranil Basak, Patil KS, Alves G, Larsen JP, et al. (2015) Parkinson’s disease and age: The obvious but largely unexplored link. Experimental Gerontology 68: 33-38.
- Ryan Barmore. Types of Parkinsonism. Parkinson’s Foundation
- Himadri Shekhaar Baul, Ceera Manikandan, Dwaipayan Sen (2019) Cannabinoid receptor as a potential therapeutic target for Parkinson’s Disease. Brain Research Bulletin 146: 244-252.
- Ivy N Miller, Alice Cronin-Golomb (2010) Gender differences in Parkinson’s disease: clinical characteristics and cognition. Mov Disord 25(16): 2695-2703.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.