Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Copper Toxicosis in A Toxicologist
*Corresponding author:Steven D Holladay, Department of Biomedical Sciences, College of Veterinary Medicine, University of Georgia, 501 DW Brooks Drive, Athens, GA 30602, USA.
Received: January 26, 2024; Published: February 20, 2024
DOI: 10.34297/AJBSR.2024.21.002865
Abstract
This report is from a 66-year-old toxicologist who developed several health problems shortly after relocating into a 30-year-old ranch-style house closer to family. These health conditions were assumed to be independent, age-related, and things to manage as best possible. Shortly thereafter, the appearance of green tinting in his all-white hair suggested excessive exposure from an unknown source to the metal copper. This occurrence also fostered the realization that each of the seemingly unrelated new health problems was a recognized symptom of copper toxicosis. Testing the household water showed 373% of the EPA recommended maximum safe level for drinking water. This case report, written by the patient, describes copper toxicosis in a human that may have been a challenging diagnosis had white hair not provided a visual indication of the metal exposure.
Keywords: Copper toxicity, Metal toxicity, Neurotoxicity, Hematotoxicity, Parkinson’s disease, Parkinson’s-like disease
Abbreviations: CNX: Cranial nerve 10 (vagus nerve); CT: computed tomography; EPA: Environmental Protection Agency; GI: Gastrointestinal; P: Primary; S: Secondary
Introduction
The author (SH) is a toxicologist who works in the academic sector. He purchased and began occupying a ranch-style house in October of 2019. The house was built 30 years earlier in 1989. Over the 6 months after relocating he began experiencing different health problems. The first of these was peripheral signs of a developing neuropathy including numbness and tingling of feet, stiff legs, problems with balance and normal walking, shaky hands and shaky voice. The second was gastric bloating manifesting primarily in the upper left gastrointestinal (GI) quadrant, feeling like an inflated balloon placed under the ribs in that region. The third was diagnosis of macrocytosis, an abnormal enlargement of red blood cells and a type of anemia. SH, 66 years-old, viewed these as unrelated health problems manifesting with aging.
New Health Challenges
Neuropathy was evaluated by the family practice physician of SH through tests that included ability to stand with feet together and eyes closed, heel-to-toe walking of a straight line, and ability to perceive light touching in the lower legs. SH performed poorly on these tests. Symptoms of neuropathy were therefore described by the physician in the visit report, which was available online to SH (“MyChart”). SH was asked to return in 3 months for follow-up neurologic evaluation, at which time he reported a new observation of gastric bloating. Computed tomographic (CT) imaging was ordered to determine possible GI bloating causes, with colon cancer being a desired first rule-out.
The imaging detected no abnormal anatomy and was followed by colonoscopy which showed normal colon internal walls and architecture. Consultation with a gastroenterologist was next arranged, ending with prescribing of probiotics. The presence of macrocytosis was detected as part of routine blood work during the next annual physical examination and felt to likely be caused by vitamin B12 deficiency. Vitamin B12 was prescribed and red blood cells size was partially diminished after 6 months and back to normal after 12 months.
SH considered neurologic disorders that best fit his age and sex, as well as family medical history. Diseases such as multiple sclerosis and myasthenia gravis were viewed as unlikely, while early Parkinson’s disease presented as most consistent. This was not a comfortable realization in that Parkinson’s is a neurodegenerative disorder in which neuropathy progresses to debilitating and the end-stage often includes dementia.
Copper Detection
A family relative walking behind SH indicated something green was on the white hair on the back of his head. SH later used a hand-held mirror to examine his hair in a large bathroom mirror behind him. Doing so, he realized the green coloration was not on his hair, but rather was in his hair. Being a toxicologist, he recognized this as a possible sign of heavy metal exposure. Green hair tinting may also occur after use of clarifying shampoos containing acetic acid to remove hair dye coloring, or from spending considerable time swimming in pools that use chlorine sanitizing systems. Neither of the latter two applied to SH. SH requested that his wife clip some of the green-tinted hair (Figure 1).
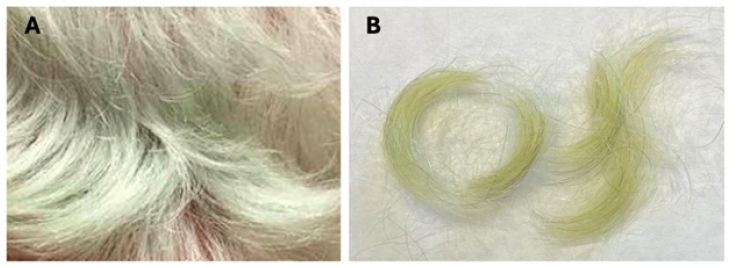
Figure 1: Figure 1A: Back of head of SH, showing green coloration of hair just above the collar. B: Clipped hair samples on white notebook paper
The most pronounced green coloration was in the occipital (lower rear) region of the scalp which may relate to hair growing faster in this region as compared to sides or top of the head. [1] During his next haircut SH asked the stylist if she could detect green tinting elsewhere in his hair, and was told the green is lighter but was distributed throughout his hair. Copper was viewed by SH as the likely causative metal, having oxidizing to green as occurs in courthouse domes in some cities (Figure 2). SH entered the house crawlspace, having not done so before, and found that he had copper plumbing pipes. This was a “light’s on” moment, with the realization occurring that metal toxicities include neurologic and hematologic signs he had recently begun expressing.
Testing Chronology
On the morning of October 27, 2020 (3 days after the weekend observation of green-tinted hair) SH collected a water sample from the faucet in his kitchen sink for metal content analysis by a University of Georgia Agricultural & Environmental Services Laboratory located at 2400 College Station Road, Athens, GA, 30605 (test results were returned November 20, 2020). This kitchen sink faucet was the one SH used for drawing drinking water. Among 14 metals analyzed all except copper were at levels determined to be safe for human exposure by the U.S. Environmental Protection Agency (EPA) (Table 1). For copper, the EPA has established a primary (P) and a secondary (S) drinking water standard. The Primary standard is a level that has been shown to cause adverse health effects, while the Secondary standard is the maximum level set for safe drinking water. Water in the sink faucet sample contained 278% of the EPA Primary standard and 373% of the secondary standard for copper. The report noted that the EPA has concluded copper levels in excess of 1.3 ppm may cause gastrointestinal distress. SH considered, prior to purchase of this house, he had started a diet that involved drinking ½ gallon of water each evening, 6-7 days/week. This practice continued throughout his time in the new house until the detection of excess copper in the household water, after which externally-purchased water was used.

Table 1: Household water metal analysis.
Note*: aThe above red type of font color for copper ppm was a part of the original report. ppm: parts per million.
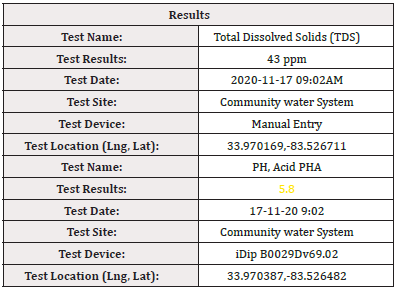
Water supplying the SH house comes from a community well that provides all 20 houses in the development. The high copper levels suggested the possibility of a non-neutral pH mobilizing copper from the copper pipe plumbing. On November 23, 2020 SH collected an additional sample of water from his kitchen sink faucet and brought it to his University of Georgia laboratory for pH determination using an Ohaus ST2200-F pH Benchtop Meter, which showed an acidic pH of 5.3 for the water. SH arranged for a plumber to examine his house and advise about methods to reduce high copper levels in the water. This person took a water sample from the entry port into the house and ran analyses that included pH (Table 2), with result of pH 5.8 (eXact iDip B0029Dv69.02 field test). The plumber cautioned SH that the water was sufficiently acidic to mobilize copper from copper pipes that hold it for different durations depending on household water-use activity (e.g., water may routinely sit in pipes for 8 or more nighttime hours). He further indicated maintaining pH in the range of 6.5-8.0 was the responsibility of the supplier to prevent this type of occurrence. SH contacted the supplier (Georgia Well & Water), described the problem and requested pH within allowable limits. SH thereafter routinely evaluated water pH using his laboratory meter, and in all cases found levels near neutral (7.0).
On January 19, 2021 SH had his household water retested for metals by the laboratory that performed the initial test. The sample contained 115% of the EPA Primary standard and 149% of the secondary standard for copper, thus had decreased considerably from levels in the initial sample but was still above EPA threshold for safe drinking. Water was tested again May 24, 2021 and contained 39% of the EPA Primary standard and 51% of the Secondary standard for copper, therefore reaching levels considered safe for human consumption by the EPA.
Copper Neurologic and Hematologic Toxicity
Altered copper homeostasis (too little copper or too much) has been associated with neurological and neurodegenerative pathologies. [2,3] High levels of copper ingestion in humans have been linked to several neurodegenerative pathologies including Parkinson’s and Alzheimer’s diseases. [4] In copper toxicosis, metal deposition in the basal ganglia of the brain is associated with development of Parkinson’s-like symptoms including dystonia (involuntary muscle contractions) and tremor. [5] Early warning signs of Parkinson's disease include shaking beginning in hands or fingers, slowed movement and rigid muscles, impaired balance, speech changes, and writing changes. [6] SH self-reported all of these symptoms to an immunologist colleague approximately 6 months before the realization he had been orally exposed to sufficient copper to cause visible greening of his white hair.
In neuropathies, long nerves extending to the periphery are typically first affected. Cranial nerve 10 (CNX), the vagus nerve, is one such long nerve as it travels from brainstem to structures that include the gut where it plays a role in peristalsis. [7] As a consequence, gastrointestinal bloating disturbances are often among symptoms displayed in patients with neuropathy. [8] Heavy metal poisoning is also associated with hematologic disorders, with copper among the metals most commonly linked to hematotoxicity [9].
Conclusion
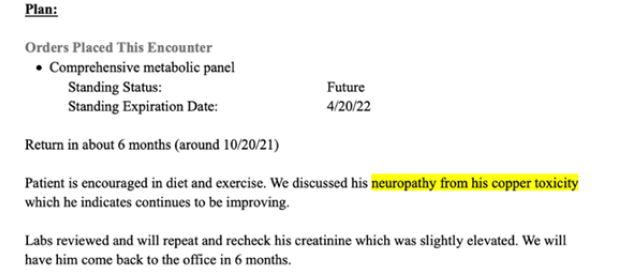
Greater than 2 years and routine haircuts (approximately every 5 weeks) were required for green coloration to disappear from the hair of SH. Over this same period of time, he described his neuropathy during visits to his physician as not appearing to be worsening, and possibly showing some level of reduced tingling and increased sensation to his feet. During a routine physician visit on April 20, 2021 SH indicated a belief that neuropathy symptoms in his legs and hands were in fact somewhat reduced (Figure 3), and that gastric bloating had also diminished.
Case reports describing symptoms of copper toxicity are rare in the literature. This is the first report describing multiple adverse health events that had the appearance of being copper toxicity-related, and were personally experienced by a toxicologist. If the toxicologist did not have white hair, he and his physician agreed the apparent underlying heavy metal cause of the neurotoxicity may have been challenging to determine. Such a missed diagnosis would have resulted in continued consumption of the contaminated water and predictable progressing of Parkinsonian symptoms. Such symptoms in this case would have been felt to have underlying etiologies for which a simple intervention was less possible.
Acknowledgements
The author is the sole contributor.
No external funding was associated with this report.
Conflict of Interest
The author has no financial or other conflicts of interest.
References
- Van Neste D (2004) Thickness, medullation and growth rate of female scalp hair are subject to significant variation according to pigmentation and scalp location during ageing. Eur J Dermatol 14: 28-32.
- Baldari S, Di Rocco G, Toietta G (2020) Current biomedical use of copper chelation therapy. Int J Mol Sci 21(3): 1069.
- Bisaglia M, Bubacco L (2020) Copper ions and Parkinson’s disease: Why is homeostasis so relevant? Biomolecules 10(2): 195.
- Desai V, Kaler SG (2008) Role of copper in human neurological disorders. American J Nutr 88: 855S-858S.
- Caudle WM (2017) Occupational metal exposure and Parkinsonism. Adv Neurobiol 18: 143-158.
- Forero-Rodriguez LJ, Josephs-Spaulding J, Flor S, Pinzon A, Kaleta C, et al. (2021) Parkinson’s disease and the metal-microbiome-gut-brain axis: A system toxicology approach. Antioxidants 11(1): 71.
- W L Neuhuber, Berthoud H-R (2021) Functional anatomy of the vagus system – emphasis on the somato-visceral interface. Auton Neurosci
- Moors VJ, Graveran KD, Shahsavari D, Parkman HP (2022) A cross-sectional study describing neuropathy in patients with symptoms of gastroparesis: associations with etiology, gastrointestinal symptoms, and gastric emptying. BMC Gastroenterol 22: 315.
- Ringenberg QS, Doll DC, Patterson WP, Perry MC, Yarbro JW, et al. (1988) Hematologic effects of heavy metal poisoning. South Med J 81: 1132-1139.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.