Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Therapeutic Modalities in Metastasis Granular Cell Tumor: A Case Report of Anal Region
*Corresponding author: Hajar ouahbi, Atlas, Provincial hospital center, Nador, Morocco.
Received: April 27, 2023; Published: August 05, 2024
DOI: 10.34297/AJBSR.2024.23.003094
Abstract
Background: The clinical evolution and biology of Granular Cell Tumors (GCT) are poorly understood, and treatment remains an issue of discussion. The is a rare benign tumor of Schwann cell origin with only 2% of them are malignant. The present case study describes the therapeutic modalities in the recurrent and metastatic situation GCT.
Case Presentation: Our case describes a 50-year-old woman who had undergone surgical excision for GCT of the anal region 4 years ago. Readmitted for local and distant relapse.
Conclusions: We believe that wide local excision is the best treatment for both benign and malignant tumors. The role of chemotherapy and radiotherapy in malignant GCT should be studied. All patients with GCT should receive follow-up to check for recurrence and metastasis.
Keywords: Granular cell tumor, Recurrent, treatment
Introduction
A Granular Cell Tumour (GCT) is a rare, benign, soft tissue tumour [1] that likely arises from Schwann cells [2]. Although it was initially classified as a myoblastoma, recent studies agree that it is more likely to be neural in origin [2,3]. Granular cell tumors may be located anywhere in the body; however, the gastrointestinal tract is infrequently involved, and anal granular cell tumors are rare [4,5]. Fanburg-Smith, et al., postulated the presence of three or more of these factors that indicate likely metastasis [6]. Metastases are more common with recurrence of a previously benign lesion spreading via lymphatic or hematogenous dissemination to the lung, liver, bone and lymph nodes [7,4]. We report here on a rare case of GCT perianal recurrent and metastasis, with discuss the most therapeutic modalities described in the literature.
Case Report
A 55-year-old woman presented with one year history of the presence of a painless mass on the anal region, on which diagnosis of GCT perianal is confirmed, patient has a surgical excision without radiotherapy or chemotherapy adjuvant. 4 years later, this patient arrived at a hospital with a painless mass on the anal region (Figure 1), the thoraco-abdominal and pelvic CT scan showing the presence of a right anal and para-anal mass measuring 130*81mm extended to the surrounding soft tissues and infiltrating the neighboring muscular structures on the right side and the perineal and buttock skin (Figure 2) with pulmonary metastasis.
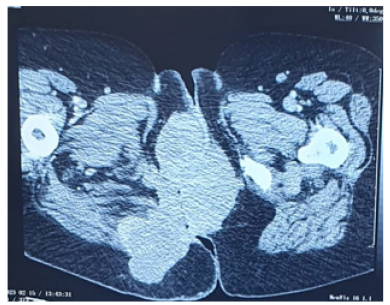
Figure 2: CT scan showing the presence of a right anal and para-anal mass measuring 130*81mm extended to the surrounding soft tissues and infiltrating the neighbouring muscular structures on the right side and the perineal and buttock skin.
The patient benefited from a discharge stoma with a new biopsy of the mass confirming the diagnosis of GCT. Pathological examination of the biopsy specimen had revealed a diffuse proliferation of large cells. These cells have a polygonal oxyphilic granuspecimensm and a regular hyperchromatic, often pyknotic nucleus. The tumoral stroma was essentially fibrous without an inflammatory infiltrate. No mitotic activity or necrosis was observed. The proliferation locally invades skeletal muscle. The cells have a PAS+ cytoplasm in histochemical study. On immunohistochemical study, tumor cells were positive to CD68 and S100 protein. The patient had taxan-based chemotherapy, after six sessions, she progressed locally and remotely with increase in number and size of lung nodules of pulmonary metastasis, then referred to us at the Oncology Center in Nador (Morocco) for additional therapeutic care. The patient was treated with doxorubicin and ifosfamide chemotherapy, and after three sessions, a dissociated response with decreased anal mass and progression of pulmonary metastasis was observed (Figure 3).

Figure 3: Local response with disappearance of the para-anal mass after 3 courses of chemotherapy based on doxorubicin and ifosfamide.
The patient’s medical record will be discussed in multidisciplinary consultation meeting for decision of the 3rd therapeutic line. All patient details have been de-identified, and the patient provided written informed consent for treatment and publication of this report.
Discussion
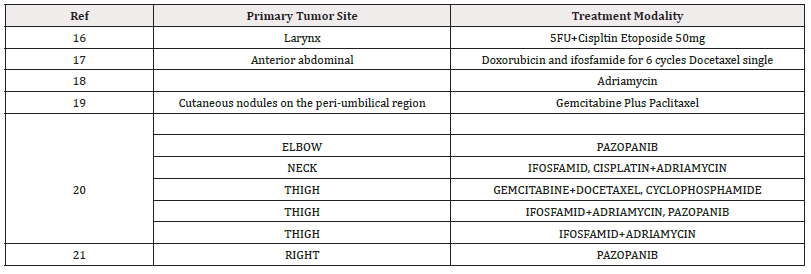
Malignant Granular Cell Tumors (MGCTs) are extremely rare sarcomas with Schwannian differentiation [8]. The tumor may be located anywhere in the body, but perianal localization is quite rare [9]. Most of the published studies present cases with local recurrence, the presence of metastasis like ours is rarely described in the literature [10]. Although the etiology and histogenesis of GCT are not completely clear, they can still be characteristic. The current gold standard for the diagnosis of GCT is histopathological and immunohistochemical examination [11]. The histopathological manifestations of GCT are characterized by a neoplastic mass with unclear boundaries in the dermis and subcutaneous tissues, including large neoplastic cells with nests or cords, and eosinophilic granules. Immunohistochemical tests often show positivity for NSE, S-100, and CD57, but some GCTs have been S-100-negative [12]. The expression of S-100 indicates that GCTs originated from Schwann cells in the neuroectoderm and expression of the macrophage marker CD68 contributes to the aggregation of lysosomes in the cytoplasm but does not reflect the origin of the tumor cells. This supports the hypothesis that GCT represents a non-specific degeneration process of mesenchymal cells via self-phagocytosis [5]. In the current case, the pathological results showed positive immunostaining for S-100 and CD68 supporting the diagnosis of a neurogenic tumor. Wide local excision is the gold standard treatment of local GCT [13,14]. Excision of affected lymph nodes is recommended in patients with lymphatic involvement [4]. The current clinical opinion is to treat the condition in line with the sarcoma-based protocol [15]. Aksoy, et al., revealed in eleven patients that chemotherapy and/or radiation did not alter the disease survival or overall survival in patients with etastasis or recurrence [16]. We report on this Table 1 some clinical cases reported in the literature, and which had a medical treatment with a response in most cases (Table 1) [17-21].
Malignant GCT is believed to be an aggressive chemo refractory disease. Recently, Vatsala Katiyar and AL [22] reported a case of malignant GCT recurrent which pazopanib monotherapy achieved a response; this was like the experience recorded for pazopanib monotherapy in the other studies [21,22,23]. Pazopanib is an oral, small molecule inhibitor of vascular endothelial growth factor receptor 1, 2 and 3, platelet derived growth factor receptor α and β, and c kit, which has shown single agent activity in patients with advanced soft tissue sarcomas [24,25] III study of pazopanib in advanced soft tissue sarcoma included one patient with a malignant GCT who experienced stable disease and tumor shrinkage [25].
Conclusions
The rarity of MGCT makes it difficult to have set standard treatment protocols. Follow-up guidelines are needed, although annual follow-up is advised to rule out local recurrence or metastatic spread. Better characterization of the genetics and driver mutations can help tailor and personalize therapy for patients. Further studies are required to clearly identify the benefits of pazopanib and other chemotherapy regimens.
Acknowledgements
None.
Conflict of Interest
None.
References
- Elkousy H, Harrelson J, Dodd L, Martinez S, Scully S (2000) Granular cell tumors of the extremities. Clin Orthop Relat Res (380): 191-198.
- Torrijos Aguilar A, Alegre de Miguel V, Pitarch Bort G, Mercader García P, Fortea Baixauli JM (2009) Cutaneous granular cell tumor: a clinical and pathologic analysis of 34 cases. Actas Dermosifiliogr 100: 126-132.
- Rekhi B, Jambhekar NA (2010) Morphologic spectrum, immunohistochemical analysis, and clinical features of a series of granular cell tumors of soft tissues: a study from a tertiary referral center. Ann Diagn Pathol 14: 162-167.
- Cohen MG, Greenwald ML, Garbus JE, Zager JS (2000) Granular cell tumor-a unique neoplasm of the internal anal sphincter: report of a case. Dis Colon Rectum 43(10): 1444-1446.
- Jianhua Ma, Yicheng Cheng, Xue Li, Wei Liu, Renghai Liu, et al. (2021) Rare case of granular cell tumor of perianal region: a case report and literature review, J Int Med Res 49(1): 300060520982689.
- Fanburg Smith, Meis Kindblom JM, Fante R, Kindblom LG (1998) Malignant granular cell tumor of soft tissue: diagnostic criteria and clinicopathologic correlation, Am J Surg Pathol 22(7): 779-794.
- Ribeiro SPP, Levy SF, Corrêa FM (2015) Granular cell tumor of rectal submucosa: case report. J Coloproctol 35: 124-127.
- Fanburg Smith JC (2013) Malignant granular cell tumour. In: Fletcher CDM, Bridge JA, Hogendoorn PCW, Mertens F (eds) WHO classification of tumours of soft tissue and bone, 4th IARC Press Lyon 190.
- Takaaki Fujii, Hiroki Morita, Satoru Yamaguchi, Soichi Tsutsumi, Takayuki Asao, et al. (2014) A Rare Case of Granular Cell Tumor of the Anal Region: Diagnostic Difficulty to Masses in the Anal Area. Int Surg 99(1): 45-47.
- Geoffrey Williams, Carlos Neblett, Shereika Warren, Garfield Blake (2021) A case of metastatic malignant granular cell tumour of the scalp. J Surg Case Rep 2021(4): rjab145.
- Cui Y, Tong SS, Zhang YH, Hui Ting Li (2018) Granular cell tumor: a report of three cases and review of literature. Cancer Biomark 23(2): 173-178.
- Solomon LW, Velez I (2016) S-100 Negative granular cell tumor of the oral cavity. Head Neck Pathol 10(3): 367-373.
- Al Bouzidi A, Choho K, Cherradi N, M Rimani, A Harket, et al. (2003) Benign granular cell anal tumor. Presse Med 32: 221-222.
- Wan XY, Hu B, Zhou ZY, Huang Y, Ren DL (2014) Recurrent granular cell tumor of the anal-perianal region: how much anal sphincter can be resected? Tech Coloproctol 18: 597-600.
- Peter S, Olencki T (2012) Unusual cutaneous malignancies. Section 9: Cutaneous Malignancies, Textbook of Uncommon Cancer, Fourth Edition John Wiley & Sons Inc P.
- Sercan Aksoy, Huseyin Abali, Saadettin Kilickap, Hakan Harputluoglu, Mustafa Erman (2006) Metastatic granular cell tumor: A case report and review of the literature, Acta Oncologica 45(1): 91-94.
- Yara A, Khaled Ali AH, Samir S Amr (2019) Alnashwan Metastasizing Malignant Granular Cell Tumor (Abrikossoff Tumor) of the Anterior Abdominal Wall, with Prolonged Survival. Case Rep Pathol 2019: 9576487.
- T Khansur, L Balducci, M Tavassoli (1987) Granular Cell Tumor, Clinical Spectrum of the Benign and Malignant Entity, Cancer 60(2): 220-222.
- Kanat O, Yalcinkaya U, Akbunar T, Kurt E, Evrensel T, et al. (2008) Gemcitabine Plus Paclitaxel may be a Promising Chemotherapy Regimen for Metastatic Granular, Cell Tumour. Clin Oncol (R Coll Radiol) 20(1): 93-96.
- Jungo Imanishi, Yasuo Yazawa, Tsuyoshi Saito, Michio Shimizu, Hiroyuki Kawashima, et al. (2016) Atypical and malignant granular cell tumors in Japan: a Japanese Musculoskeletal Oncology Group (JMOG) study Int J Clin Oncol 21(4): 808-816.
- Sachi Morita, Mariko Hiramatsu, Mihoko Sugishita, Bishal Gyawali, Takashi Shibata, et al. (2015) Pazopanib monotherapy in a patient with a malignant granular cell tumor originating from the right orbit: A case report. Oncol Lett 10(2): 972-974.
- Katiyar V, Vohra I, Uprety A, Wei Yin, Shweta Gupta (2020) Recurrent Unresectable Malignant Granular Cell Tumor with Response to Pazopanib. Cureus 12(5): e8287.
- Conley AP, Koplin S, Caracciollo JT, Damon R Reed, Nicolas P Webber, et al. (2014) Dramatic response to pazopanib in a patient with metastatic malignant granular cell tumor. J Clin Oncol 32(32): e107-e110.
- Sleijfer S, Ray Coquard I, Papai Z, Axel Le Cesne, Michelle Scurr, et al. (2009) Pazopanib, a multikinase angiogenesis inhibitor, in patients with relapsed or refractory advanced soft tissue sarcoma: a phase II study from the European organisation for research and treatment of cancer soft tissue and bone sarcoma group (EORTC study 62043). J Clin Oncol 27(19): 3126-3132.
- Van der Graaf WT, Blay JY, Chawla SP, Dong Wan Kim, Binh Bui Nguyen, et al. (2012) Pazopanib for metastatic soft tissue sarcoma (PALETTE): a randomised, double blind, placebo-controlled phase 3 trial. Lancet 379(9829): 1879-1886.




 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.