Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Sino-nasal T/NK lymphomas (Medio-Facial Malignant Granulomas)
*Corresponding author: Jbali Souheil, Departments of ENT and Maxilla-Facial Surgery La Rabta, Cervico-Facial Carcinology Surgery: Salah Azaiez Institute, Tunisia.
Received: April 08, 2019; Published: May 15, 2019
DOI: 10.34297/AJBSR.2019.03.000627
Abstract
Nasal T / NK Lymphoma Was First Described In 1933 As A Medio-Facial Malignant Granuloma. The Diagnosis of This Rare Disease Is Clinical and Immuno-Histopathological. We Report 18 Cases of TNK Lymphoma Collected at ENT and Maxillo-Facial Surgery Department Of La Rabta Hospital Over A Period Of 17 Years (2000-2016). We Included in This Work All Patients Whose Diagnosis of TNK Lymphoma Was Confirmed Histologically and By an Immuno-Histochemical Study. The Classification Adopted Was That of The World Health Organization (WHO) For Lymphoma (2008). The Treatment Was Based on Exclusive Radiotherapy for Four Patients Classified Stage IE, Radio-Chemotherapy for Five Patients: All Classified Stage IE Diffuse, And One Patient Classified Stage IV. Exclusive Chemotherapy Was Performed in Four Patients: Classified Stage IIE In Three Cases and Stage IE Diffuse in One Case. The Mean Follow-Up of Our Patients Was 8 Months (2-42 Months). Clinical Remission Was Noted Only in Two Patients.
Keywords: T/NK Lymphoma; Nasal; Radiotherapy; Chemotherapy
Introduction
TNK Lymphoma is a Rare Pathological Entity Characterized by a Necrotic Process Starting in The Nasal Cavity, Extending to Facial Bones and Destroying Them. World Health Organization’s Classification Helped to Standardize Different Reviews of This Pathology. As Many Other Diseases, TNK Lymphoma Is Related to EBV Infection. It Keeps, Still, A Bad Prognosis Even If Current Treatments Allowed Long Remissions. Evolution Is Often Difficult to Predict and Must Search for Other Prognostic Markers Such as Cytogenetics. The Aim of Our Work Was to Describe the Epidemiological, Clinical and Therapeutic Characteristics of TNK Lymphoma Through A Retrospective Study Of 18 Cases Collected in Our Department Over A Period Of 17 Years (2000). -2016).
Methods
Mentioned Above, Our Study Was Retrospective Including 18 Patients Diagnosed with TNK Lymphoma. We Included Only Those Whose Diagnosis of TNK Lymphoma Was Confirmed Histologically and By an Immuno-Histochemical Study. The Classification Adopted Was That of WHO for Lymphoma (2008). We Collected and Analyzed All Information Available in Medical Files, Including All Epidemiological Data, Complementary Examinations and Therapeutic Modalities. Given Its Retrospective and Observational Nature, This Work Was Not Subject to Prior Consent of Patients Included in It. We Declare That We Have No Conflict of Personal Interest Incompatible with The Objectives of This Work.
Results
The mean age of our patients was 51 years old (35-81 years). A frequency peak was noted in the age group 40 - 50 years old. A male predominance was, also, noted with a sex ratio of five (15 males / 3 females). The mean diagnosis delay was 6 months (1- 18 months). A history of hypertension was found in two patients and diabetes in three patients. Nasal obstruction was the main complaint reported by 15 patients: unilateral in 11 cases and bilateral in four cases. Other symptoms were purulent rhinorrhea: 11 cases; spontaneous epistaxis: 11 cases; cacosmia: five cases; otalgia, sensation of ear fullness and unilateral hearing impairment: four patients. Ophthalmologic complaints were reduced visual acuity in two cases and blindness in one case. Headaches, impaired general condition and prolonged fever were reported in eight, seven and four cases respectively. Physical examination found facial deformities in 11 patients: mandibular and jugal swelling in one and four cases respectively, hemi-face edema in four cases and nasal pyramid deformity in four cases. Unilateral exophthalmia was also found in four cases associated to chemosis in one case.
All patients have had a nasal endoscopy, which objectified a tumor located in the nasal cavity in 17 cases and in the cavum in one case. Examination of the oral cavity showed necrotic ulceration of the hard palate mucosa in three cases performing an oro-nasal communication in one case. Neck examination found adenopathies in five cases: unilateral in two cases and bilateral in three cases. They were hard and fixed in three cases. They were located in the lymph node groups II, IV and V in three cases, group II in one case and groups II and V in one case. Neurological examination revealed a paralysis of cranial nerve pairs II, III, IV and V in two patients, paralysis of left VI in one patient and of V cranial nerve in one case. A facial bone CT scan was performed for all patients (Figure 1). It objectified a sino-nasal tumoral process and evoked the diagnosis of TNK lymphoma in two cases.
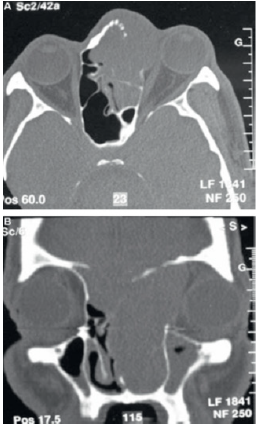
Figure 1: Non-injected facial bones CT scan: axial and coronal sections: lysis of the medial wall of the orbit and upper wall of the left frontal sinus with orbital and endo-cranial extension.
This tumor was located in nasal cavity in 17 cases with extension to ethmoid in seven cases, maxillary sinus in six cases, sphenoid sinus in one case, cavum in two cases, oral cavity in two cases and to oropharynx in three cases. It was located in the cavum in one case. An orbital extension through an orbital lamina break in was found in four cases. A cerebral CT scan, performed in two cases, showed intracranial extension with mass effect on frontal lobe. Extension to soft tissues was observed in six cases including buccal mucosa in four cases, pre-mandibular and frontal soft tissues in one case for each one. A total body CT scan was performed in nine cases as part of distant extension assessment. It was normal in five cases. It revealed the presence of mediastinal lymphadenopathies in four cases. All patients have had a tumoral biopsy. Histologic description showed a chorion occupied by lymphomatous proliferation made of medium to large cells with clear cytoplasmic. In places, the tumor cells were arranged in perivascular sheaths (angiocentric) destroying the vascular wall (angio-destructive) with hemorrhagic suffusions and tumor necrosis. Immuno-histochemical study showed in all cases an intense and diffuse cytoplasmic positivity of tumor cells to anti-CD3 antibody and their negativity to anti-CD20 antibodies and to cytokeratin.
The CD56 antibody, performed for all patients, was positive while CD30 (achieved in 12 cases) was positive in only seven cases. Clinical and para-clinical assessment allowed to classify the tumor as follows (according to Ann Arbor classification): stage IE in 12 cases (67%) and stage IIE in four cases (22%) and IV in two cases (11%). Two patients were lost to sight and five died before any therapeutic approach. Treatment was based on exclusive radiotherapy for four patients classified IE stage. Combined treatment (radiotherapy and chemotherapy) was performed in five cases classified as diffuse IE stage and in one patient with stage IV disease. Chemotherapy was performed in four patients classified stage IIE in three cases and stage IE diffuse in one case. The mean follow-up of our patients was 8 months (2-42 months). Only two patients were in clinical remission. The evolution was marked by the death of 12 patients and four patients were lost during follow-up. Seven patients underwent an imaging control (CT scan): four were in clinical remission and the scanner was without abnormalities. Two of these patients were, later, lost to follow-up.
Discussion
Sino-nasal TNK lymphomas are rare. They are more common in Asia, Mexico and South America. In Tunisia, their frequency is unknown [1]. TNK lymphoma accounts for 45% of primary nasal lymphomas [2]. It associates ulcerative-necrotic lesions preferentially starting in the nasal cavities and sinuses (70%). It can also develop in the Waldeyer’s ring (38%), oral cavity (14%), larynx, hypopharynx (10%) and even in the mandible or cheek [3]. T / NK lymphoma can be seen at any age but mainly affects subjects in the fourth and fifth decade [4]. The average age of our patients was 51 years old. It often affects male subjects [2,5]. In our study, the sex ratio was five. T / NK lymphoma has an unknown pathogenesis. However, it is strongly associated with EBV infection [1,6]. This EBV infection is associated with a poor prognosis with frequent local relapses, possibility of extension outside lymph nodes territories and appearance of macrophage activation syndrome [5]. Detection of EBV in almost all tumor cells allows for tumor proliferation of cytotoxic phenotype to make the diagnosis in cases of unusual clinical presentation [6].
Some studies have linked these lymphomas to overexpression of the P53 protein, associated or not with P53 gene mutation (often induced by the presence of EBV) [8,9]. The mean diagnosis delay is often prolonged because of the chronicity of lesions and absence of specific revelation mode [10]. The majority of patients presented with localized lesions but often with invasion of nearby structures such as: face sinuses, palate and nasal cavities [11]. Patients often present with unilateral nasal obstruction, which is initially intermittent, and then permanent associated with fetid rhinorrhea. Smell disorders can also be present [1]. In 20 to 40% of cases, clinical presentation may be distorted by a generalized granulomatosis affecting skin, subcutaneous tissues, eyes, gut, lungs and nervous system [12]. A large number of biopsy specimens are necessary in order to diagnose nasal T / NK lymphoma. In fact, this tumor is often site of necrotic and hemorrhagic rearrangements and biopsies may only cover areas of remodeling [13]. Histological examination shows layers of atypical cells of variable size. Mitoses are frequent. What characterizes the nasal T / NK lymphoma is the presence of vascular lesions with tumor cells placed in perivascular cuffs (angiocentrism), with penetration of these cells into the vascular wall and lumen forming, sometimes, vascular thrombi (angiodestructive lesions).
Areas of necrosis and fibrosis are observed, with pseudoepitheliomatous hyperplasia of the nasal mucosa [14,15]. Immunophenotypic study reveals the expression of cellular markers of T lymphocytes and of NK lymphocytes, hence the name of this lymphoma: TNK lymphoma. Typical immune-phenotype of this lymphoma is CD2+, CD56+ (which is the NK-specific marker), expression of intracytoplasmic anti-CD3 antibody with surface CD3 negativity [16]. EBV can be found in tumor cells in the vast majority of cases as confirmed by several immuno-labeling and molecular biology studies [17]. According to Rodriguez, therapeutic innovations must be tried, including immunotherapy, which targets the expression of EBV; EBV infection is associated with 90-100% of TNK lymphoma cases inducing a poor prognosis [18]. As all sino-nasal tumors, CT scan remains the first complementary exploration [1]. It allows to precise tumor localization, extension to around structures and other informations such as bone lysis. It is also essential for evaluation of therapeutic response and followup thereafter [19]. MRI allows evaluating tumor relation with cerebro-meningeal structures. In fact, it can differentiate between inflammation, soft tissues edema and tumor infiltration. Tumor appears iso-intense compared to muscles in T1 sequence and moderately hyper-intense in T2 sequence.
This treatment is based on radiotherapy and chemotherapy. Their use, separately or in combination, has been subject of several studies. Indications depend on the stage of the disease and therefore on the extension assessment. For localized stages (stages I and II), external radiotherapy with a minimum dose of about 52 Gy (conventional fractionation) is recommended. It gives a complete remission in 40 to 80% of cases and an overall survival at five years between 40 and 59% [22]. For advanced stages greater than IIE and stage B, radio-chemotherapy combination could significantly improve survival [23]. According to Mikhaeels and Spittle, intensive chemotherapy is necessary even in localized stages given the aggressiveness of this type of lymphoma [24]. This tumor has a poor prognosis: five-year overall survival varies between 10 and 45% [25].
Conclusion
T/NK lymphoma has benefited from advances in diagnostic and therapeutic means. It keeps, however a bad prognosis. The current challenge is to standardize therapeutic protocols to optimize survival rates and improve management. As future perspectives are discussed immunotherapy and targeted molecular therapy focused on EBV infection frequently observed.
Conflicts of Interests
No.
References
- Forcioli J, Meyer B, Fabiani B (2005) Granulome malin centrofacial. Encyclopédie médicale d’Otorhinolaryngologi 2(4): 390-400.
- Amaoui B, Saadi I, Sifat H (2003) lymphoma angiocentrique de la face à propos de 2 cas. Cancer Radiothérapie 7(5): 314-316.
- Susarla M, Sharaf A, Faquin W (2010) Extranodal natural killer Tcell lymphoma, nasal type with minimal osseous involvement: report of a case and literature review. J Oral Maxillofac Surg 68(3): 674-681.
- Mestiri S, Zeglaoui I, Sriha B (2008) Extra-nodal T, lymphomas of the nasal cavities and sinuses. Ann Otolaryngol Chir Cervicofac 125(4): 188- 192.
- Al-Hakeem DA, Fedele S, Carlos R (2007) Extranodal NK/T-cell lymphoma, nasal type. Oral Oncol 43: 4-14.
- Charalambos C, Solamids MD, Miller A (2002) Lymphomas of the oral cavity: histology, immunologic type and incidence of Epstein Barr Virus Infection. Hum Pathol 33(2): 153-157.
- Tian C, Wang Y, Zhu L, Yu Y, Zhang Y (2015) Primary bone natural killer/ T cell lymphoma, nasal type without EBV infection: a case report. Int J Clin Exp Pathol 8(11): 14836-14839.
- Li T, Hongyo T, Syaifudin M (2000) Mutation of the p53 gene in nasal NK/T-cell lymphoma. Lab Invests 80(4): 493-499.
- Huang WT, Huang CC, Weng SW, Eng HL (2009) Expression of the multidrug resistance protein MRP and the lung-resistance protein LRP in nasal NK/T cell lymphoma: further exploring the role of P53 and WT1 gene. Pathology 41(2): 127-132.
- Kyrmizakis DE, Hajiioannou JK, Koutsopoulos AV (2006) Primary nasal non-Hodgkin lymphomas presented initially as benign disease. Am J Otolaryngol 27(3): 217-220.
- Ladeb S, Gaulard P, Ben Othmen T (2003) Nasal NK/T lymphoma. A case report Ann Pathol 23: 149-152.
- Kaluza V, Rao DS, Said JW (2006) Primary extranodal nasal-type natural killer/T-cell lymphoma of the brain: a case of report. Hum Pathol 37(6): 769-772.
- Ladeb S, Gaulard P, Ben Othmen T (2003) Nasal NK/T lymphoma. A case report Ann Pathol 23: 149-152.
- Costes V (2009) Pathologie lymphoïde de la tête et du cou. Ann Pathol 29(4): 323-334.
- Abdullah D, Fedele S, Carlos R (2007) Extranodal NK/T cell lymphoma nasal type. Oral Oncol 43(3): 4-14.
- Hmidi M, Kettani M, Elboukhari A, Touiheme N, Messary A (2013) Lymphome TNK nasosinusien. Annales francaises d’oto-rhinolaryngologie et de pathologie cervico-faciale 130(1): 149-152.
- Liang X, Graham DK (2008) Natural killer cell neoplasms. Cancer 112(7): 1425-1436.
- Chetcha Chemegni B, Hulin C, Feuget P, Bordigoni D, Lederlin P (2012) Les Lymphomes T-NK extraganglionnaire de type nasal: expérience du CHU de Nancy à propos de 9 cas. Health Sci 13(2): 155-160.
- Kharoubi S (2005) Tumeurs malignes des fosses nasales à propos de 21 cas. Cancer Radiother 9: 187-195.
- Zhou X, Lu K, Geng L, Li X, Jiang Y, et al. (2014) Utility of PET/CT in the diagnosis ans satging of extranodal natural killer/T-cell lymphoma: a systematic review and métanalysis. Medecine (Baltimore) 93(28): e258.
- Ramsay A, Rooney N (1993) Nasofacial T-cell lymphoma. Eur J Cancer B Oral Oncol 29B(2): 99-102.
- You JY, Chi KH, Yang MH (2004) Radiation therapy versus chemotherapy as initial treatment for localized nasal natural killer (NK)/T-cell lymphoma: a single institute survey in Taiwan. Ann Oncol 15(4): 618- 625.
- Zhang L, Jiang M (2016) Five-year analysis from phase 2 trial of « sandwich » chemoradiotherapy in newly diagnosed, stage IE to IIE, nasal type, extranodal natural killer/T-cell lymphoma. Cancer Med 5(1): 33- 40.
- Armitage JO (2016) Peripheral T-cell lymphomas: their time has come. Oncology (Williston Park) 23(13): 1151-1152.
- Lee J, Park YH, Kim WS (2005) Extranodal nasal type NK/Tcell lymphoma: elucidating clinical prognostic factors for risk-based stratification of therapy. Eur J Cancer 41(10): 1402-1408.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.