Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Antimicrobial Resistance: “The Threat of Future Health”
*Corresponding author: Aikaterini Frantzana, Department of Health Sciences, European University of Cyprus, Greece.
Received: August 19, 2019;Published: August 26, 2019
DOI: 10.34297/AJBSR.2019.04.000850
Abstract
Introduction: Antimicrobial resistance (AMR) is now a major issue in healthcare. Antibiotics may be used for the treatment of fungus and parasites. They are applied in veterinary and food chemistry except for Medicine.
Purpose: The purpose of this article is the detailed assessment and prevention of antimicrobial resistance in hospitals and the community after the indiscriminate use of antibiotics.
Methodology: The manuscript consists of a thorough scrutiny of both international and Greek research and review studies regarding antimicrobial resistance and national action plans.
Results: The emergence of antimicrobial resistance to antibiotics constitutes a huge threat for human health. Moreover, it is a paramount European and global concern involving scientific providers. Recognizing the severity of the situation, the government established a series of measures to raise awareness among all those involved and curb the consumption of antimicrobial drugs
Conclusions: A holistic approach with prudent and rational use of antimicrobial agents is required in order to reduce AMR and hospitalacquired infections.
Introduction
The use of the first antibiotics took place about 2,500 years ago by the ancient Chinese in their attempt to cure various human diseases caused by bacteria [1]. In 1928 Alexander Fleming discovers penicillin and sets the basis to produce the first antibiotics in 1943 [2]. Antibiotics are currently considered chemotherapeutic drugs that are used to treat or prevent infections caused by bacteria and can kill or inhibiting the growth of pathogenic microorganisms. Antibiotics can be used to treat fungi and parasites, but they are not effective against viruses. Thanks to their application, the threat of infectious diseases has been significantly reduced, but over the years, and frequent use, bacteria have acquired resistance to antibiotics. This has resulted in many hospital infections, infections of various systems in the body and sexually transmitted infections [3]. Seventy years later, antimicrobial resistance (AMR) is recognized as a serious threat to public health, and according to World Health Organization (WHO) data, deaths associated with resistant microbial infections amount to 25,000 per year for the European Union and 23,000 for the US and the annual cost of inhospital infections is about $33.8 billion and €7 billion respectively.
By 2050, ten million more people are expected to die due to antimicrobial resistance, and one hundred trillion dollars will have been spent with a 2%-3.5% reduction in international gross product [4]. Greece is one of the first countries in Europe for the resistance of microbes to antibiotics, and it is estimated that three thousand deaths are due to in-hospital infections, while the cost is over 1.5-2.5 billion euros per year [5]. According to the latest publications of the European Surveillance of Antimicrobial Consumption (ESAC), our country also shows a gradual increase in non-hospital antibiotic consumption from 1997 (25.06 DID) to 2005 (34.73 DID) (DID: Daily Dose per 1000 inhabitants per person day), while in 2008 it reached levels of 45 DDD (DDD: Defined Daily Dose) levels almost double that of other European countries [6]. At the same time, over-consumption of antibiotics, with much of the primary care, brings us back to the top with a prescription rate of 36.1 per 1,000 people when the average in OECD countries is 20.6 per 1,000 people. France ranks second, with a proportion of 29.9 people per 1,000 the last in the consumption of antibiotics is the Dutch, with just 10 out of 1,000 taking antibiotics. Although antibiotic prescribing improved in 2016, consumption continues to remain high, with the largest share in the supply of antibiotics without a prescription from the public [7].
Aim
The purpose of the review article is the detailed assessment and prevention of antimicrobial resistance in hospitals and the community after the indiscriminate use of antibiotics.
Methodology
The manuscript consists of a thorough scrutiny of both international and Greek research and review studies regarding antimicrobial resistance and national action plans. The key words used are: antibiotics and antimicrobial resistance. The language of the manuscripts searched was the criterion for exclusion except for Greek and English.
Speaking about antimicrobial resistance
The increasing use of antibiotics is a major problem in Public Health as it leads to multiple and insoluble problems, increasing antimicrobial resistance and complicating the treatment of infections [8]. The Ministry of Health, recognizing the gravity of the situation, has introduced a series of measures to resolve the issue, the aim of the campaign is to raise awareness among all concerned to limit the consumption of antimicrobial drugs. These efforts concern:
a) The reduction of in-hospital infections. These infections occur 48 to 72 hours from the patient’s introduction, are “Iatrogenic adverse events” and together with antimicrobial resistance are indicators of quality of health services provided [9]. Most infections occur in Intensive Care Units (ICUs) (54.9%), in pathology clinics (27.4%) and in surgical clinics (17.7%). Mortality is recorded 28 days after the first positive culture and escalates over 35.7% [10]. In Greece, a legal framework for dealing with infections has been applied since 2014; it requires mandatory monitoring, compliance with internal rules and regulations of prevention and establishment of Hospital Infections Committees [11]. Antimicrobial Stewardship forces all Health Professionals to administer medicines based on guidelines. The reason is that scientific research no longer produces new antibiotics at the rate required by the increasing resistance of pathogenic microorganisms. The prolongation of the lifetime of existing antibiotics is imposed to be obeyed and their rational use to be promoted so as the antimicrobial resistance to be as little as possible [12].
b) The ban on the sale of antibiotics without a prescription About 15% of total antibiotic consumption comes from their sales through nonprescription medication and one in three Greeks has antibiotics at home and uses them, resulting in the development of microbial resistance [13]. Over time and as the resistance to last-line antibiotics increases, we are faced with a terrible future in which we will not be able to perform any routine surgery [14].
c) Restriction of antibiotics in non-medical areas. The reckless use of antibiotics is not only applicable to medicine but is found in livestock, fish farming and agriculture. Excessive and often illegal use of antibiotics in plant breeding and animal husbandry results in resistant germs being transported through the food chain and their consumption to humans. It is found off the record that Greek individuals consume only as food antibiotics at least 10,000 tons per year. Antibiotics are currently used only for therapeutic purposes and in some cases preventively [15].
Addressing antimicrobial resistance
Managing change is a big challenge for health units and requires skills and readiness from their management. The introduction of an integrated program for the prevention, control, treatment and recording of infections in the public hospital and in the community includes [16]:
Managing change is a big challenge for health units and requires skills and readiness from their management. The introduction of an integrated program for the prevention, control, treatment and recording of infections in the public hospital and in the community includes [16]:
a) Measures, rules and procedures for the prevention and treatment of AMR as well as the control of hospital infections in each nursing unit.
b) Evaluation of the results of the implementation of measures taken with quantitative and qualitative indicators of achievement regarding the quality of the provided health services and the efficiency of the health care units. Controlling AMR levels, effects, consumption of antibiotics, and compliance by health professionals.
c) Control of AMR and Infectious Diseases in the Community as they are increasingly encountered in non-hospital settings due to non-prescription antibiotics. Compliance of pharmacists with administration of antibiotics only by prescription and online prescription control [5].
d) Control of antibiotics that are used in both Greek livestock farming and agriculture at the level of both prevention and treatment. Continuous and low doses of antibiotics in farm animals prevent the onset of disease and accelerate animal growth while increasing the AMR in humans through their consumption. In our country, since 2006, a strict legal framework is in operation to control all veterinary medicines. Furthermore, a veterinary prescription is required for their use in accordance with the Veterinary Medicines Regulations (VMR). Greece has been reporting the annual sales of antibiotics used in animal husbandry to the EU since 2017 [15].
e) Industrial investment in antibiotic production is declining due to increased expense and lack of scientific discovery, preferring to make lifelong medicines rather than producing an antibiotic to be used for a short period of time [16]. The antibiotic market is over; new research and drug discoveries are needed from industries that take a long time and a lot of investment. Therefore, in order to have new antibiotics, consumption and therefore, the resistance to microbes should be reduced again [17].
Functional levels refer to decisions taken by inferior executives. Also, they are designed to meet the goals set by senior managers. They work by setting goals, means and ways of achieving them. They draw up annual reports as regards the timetable and utilization of human resources. Also, they help to inform and educate all the involved people. Their work concerns [18]:
a) The Hospital Infection Control Committee (HICC)
b) The Antimicrobial Resistance Surveillance System (ARSS)
c) The Infection Control Committee (ICC)
d) The National Agency for Medicines and Medical Devices (NAMMD)
e) The Center for Disease Control and Prevention (CDC).
The use of antibiotics in the community has much of the responsibility for AMR; according to European Commission (Euro barometer) surveys in 2013, and in 2016, the proportion of nonprescription antibiotics increased from 5% in 2013 to 7% in 2016, with the highest rates in Greece, Romania and Cyprus without a prescription sold by pharmacies. Over-the-counter antibiotics sales are prohibited by law in all EU Member States with the aim of limiting AMR. The reasons leading to the use of non-prescription antibiotics are [19,20]:
a) The patient’s social status and education
b) The communication between the doctor and the patient
c) Pharmacists’ knowledge and attitudes
d) The lack of law enforcement and sanctions for nonprescription antibiotics.
The measures being applied to address the above issues aim at the prudent use of antibiotics by outpatients at the following levels [21]:
I. The Patient’s level: Informational and online campaigns, use of media (TV, radio, internet etc.) educational courses with seminars and programs, public awareness of the AMR problem, guidance on when to consult their doctor or pharmacist and when an antibiotic is appropriate [22].
II. Level of health care system: Media messages should also be supported by pharmacists and general practitioners who play a key role in informing the public. Pharmacists are health consultants and under no circumstances they must diagnose or suggest medication. They are required by law to carry out the online prescriptions of doctors and to offer further clarifications if necessary [23]. Doctors should be trained regarding the use of antibiotics. The cost of consulting the doctor about antibiotics helps to reduce the use of antibiotics taken without prescription and the application of Strep test to the patient reduces costs and targets at the right treatment [19].
III. Multilevel: National plans to combat AMR should further encourage the implementation of laws on the prohibition of non-prescription (OTC) antibiotics. A multi-faceted partnership is required between organizations such as the Anti-microbial Resistance and the Alliance for the Prudent Use of Antibiotics (APUA), Hanhellenic Pharmaceutical Association (PFS), EOPYY, EOF, the Ministry of Health, and HCDCP. HCDCP has a special working group, who control the rational use of antibiotics and it takes actions to inform all those involved in the use of antibiotics, prescribers and consumers every year [21].
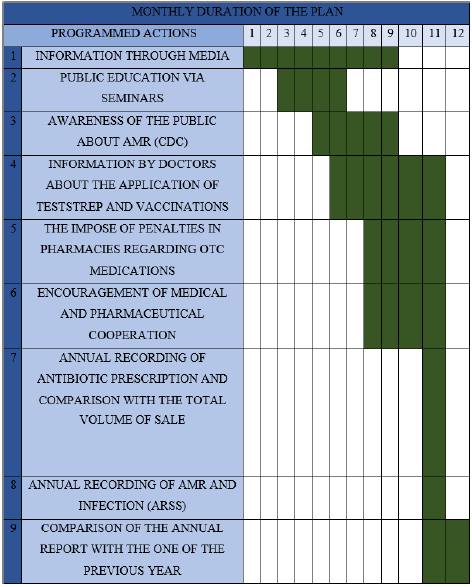
The Figure 1 shows a supposed timetable for implementing public awareness measure to reduce the use of non-prescription antibiotics (Figure 1).
Particularly, communication between healthcare professionals and patients is of importance and is extremely important in understanding the messages transmitted by the transmitter and received by the receiver [24,25]. Effective communication between healthcare professionals and patients is a dynamic alternating relationship. It is a communicative interaction between health professionals who will make a proper assessment, accurate diagnosis and choice of appropriate treatment, and patients who, through good communication, will understand the medical guidelines and work together to improve their health [26]. Effective communication begins while taking the patient’s history and affects the therapeutic effect, relying on cooperation and trust, helps reduce anxiety and externalize the feelings of the patient [18]. In this way, it aims to more effectively management of health problems, timely and valid community information on AMR and the risk of using non-prescription antibiotics [25].
Conclusion
The emergence of antibiotic resistance is an enormous threat to human health, a major European and global problem involving areas such as medicine, livestock farming and agriculture. A holistic approach to the issue is required with prudent and rational use of antimicrobial agents to reduce AMR. The creation of the proposed timetable aims to implement these measures and aims to reduce AMR in the community.
References
- Kotsiftopoulos C, Kourkouta L, Papageorgiou M (2014) The use of Antibiotic Medicine. Monograph, Lapp Lambert Academic Publishing, Germany.
- Silver L Lynn (2011) Challenges of Antibacterial discovery. Clin Microbiol Rev 24(1): 71-109.
- ECDC/EMEA (2009) Joint technical report entitled the bacterial challenge: time to react. Assessments based on bacteria most frequently isolated from blood cultures in Europe.
- WHO (2015) Global Action Plan on antimicrobial resistance.
- Papaioanidou P, Tsanakalis F, Akritopoulos P (2009) Attitudes to the use of antibiotics by the general population in Greece. Pharmacoepidemiology and Drug Safety 18(4): 253-257.
- Adriaenssens N, Coenen S, Versporten A, Muller A, Minalu G (2011) European surveillance of antimicrobial agents (ESAC): Use of antibiotics in external patients in Europe (1997-2009) Journal of Antimicrobial Chemotherapy 66: 13-12.
- HCDCP (2017) Center for Disease Control and Prevention.
- Kourkouta L, Kotsiftopoulos Ch, Papageorgiou M, Iliadis Ch, Monios A (2018) Use of antibiotics in child age-a review. Prog Health Sci 8(1): 158- 162.
- Maltese E, Kontopida F, Disease X, Katerelos P2, Gourgoulis GM et al. (2014) Action Plan to combat infections due to carbapenem-resistant, Gram-negative pathogens in acute-care hospitals in Greece. Journal of Global Antimicrobial Resistance 2(1): 11-16.
- Apostolopoulou E, Raftopoulos V, Filntisis G, Kithreotis P, Stefanidis E et al. (2013) Surveillance of Device-Related Infectious Rates and Mortality in 3 Greek Intensive Care Units. Am J Crit Care 22(3): e12-e20.
- Rockull, MD (2006) AHRQ Intra-inocuous Demonstration Quality. Indicator February Health and Quality Organization.
- OECDOC (2017)-Consumption and Antibiotic Conservation Conservation Team (OECOCHA).
- L Kourkouta (2016) Polypharmacy in Elderly. J Pharma Pharma Sci (JPPS) 103: 1-5.
- Umscheid CA, Mitchell MD, Agarwal R, Williams K, Brennan PJ et al. (2011) Assess the proportion of healthcare-associated infections that can reasonably be avoided by mortality and legal costs. Infect Control Epidemiol 32(2): 101-14.
- Gonzalez-Zorn B, Escudero JA (2012) Ecology of antimicrobial resistance: animals, food and the environment. International Microbiology 15(3): 101-109.
- Frantzana A, Charalambous M (2019) Hospital Hygiene and Safety. Am J Biomed Sci & Res 2(5): 172-176.
- OECD 23 Nov 2011 ISBN: 9789264126107 (HTML).
- Bostanitis I, Tsalidou M (2010) Patient satisfaction determinants: Doctor- patient relationships Health Inspection. 21: 15-19.
- Grigoryan L, Burgerhof JG, Degener JE, Deschepper R, Lundborg CS, et al. (2010) Attitudes, beliefs and knowledge on antibiotic use and self-medication: a comparative European study Pharmacoepidemiology and Drug Safety 16(11): 1234-1243.
- Kourkouta L, Kotsiftopoulos Ch, Papageorgiou M, Iliadis Ch, Monios A (2017) The rational use of antibiotics medicine Journal of Healthcare Communications 2(4): 1-4.
- Harris AM, Hicks LA, Qaseem A (2016) Appropriate Antibiotic Use for Acute Respiratory Tract Infections in Adults: Advice for High-Value Care from the American College of Physicians and Centers for Disease Control and Prevention. Ann Intern MedJan 164(6): 425-434.
- Holstiege J, Mathes T, Pieper D (2015) Implications of computer-assisted clinical support systems to improve the delivery of antibiotics by primary care providers: systematic review. Journal of the American Medical Association Information Technology 22(1): 236–242.
- Simo S, Fraile, D, Sanchez A (2013) Disorders of Pharmacopoeia Pharmacy. Anales de pediatria 79(1): 10-14.
- Kourkouta L, Barsamidis K, Lavdaniti M (2013) Communication skills during the clinical examination of the patients. Progress in Health Sciences 3(1): 119-122.
- Polykandrioti M (2011) Need for information and information for patients the Step of Asklepios. 10(4): 439-440.
- Kourkouta L, Papathanasiou IV (2014) Communication in Nursing Practice. Mater Sociomed 26(1): 65-67.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.