Mini Review 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Radiation Prosthesis for Improving the Life of Cancer Patients
*Corresponding author: Harisha Dewan, Department of Prosthetic Dental Sciences, Jazan University, Kingdom of Saudi Arabia.
Received: August 16, 2019;Published: August 26, 2019
DOI: 10.34297/AJBSR.2019.04.000849
Abstract
Cancer, one of the non-communicable diseases, is amongst the major public health problems in India. Radiotherapy is being used as an adjunctive form of treatment in the management of head and neck cancer. Adverse tissue reactions are associated with the use of radiotherapy in the management of patients with head and neck cancer. With a proper oral hygiene and dental care program, protective radiation prostheses can help reduce the morbidity seen with existing radiotherapy regimens.
Keywords: Radiotherapy; Radiation prostheses
Introduction
While radiotherapy for malignant tumors of the head and neck region is effective in tumor control, late complications often occur in the mouth. Side effects of concern for prosthetic dentistry are [1]: thinning of membranes and telangiectasia capillary tube extension, bone exposure and osteoradionecrosis, salivary-gland damage and fibrosis of the skin and sub membranous tissues. In addition to the use of radioprotective drugs like palifermin, benzylamine mouthwash [2], a Prosthodontist can help by the fabrication of radiation stents which can protect normal tissues from radiation injury. This article presents a review of the current applications of these devices which can help to prevent the unnecessary irradiation of surrounding normal tissues, thus reducing the severity of the reaction and throws light on their fabrication, uses and, importance.
Materials Used to Fabricate Radiation Stents
The most common material used for stent construction is heat cure acrylic resin. Cerrobend (bismuth50% lead-26.7%, tin- 13.3%, cadmium-10%) is the most commonly used shielding alloy, which has a low fusing temperature (158F) [3]. It has a melting temperature of 140 F and hence it can be melted and poured into the cavity prepared, blocked out with clay and backscatter prevented by auto polymerizing MMA resin. Cancer patients mostly are treated at 1.8-2 Gy per fraction and the treatment lasts from 4 to 7 weeks. This type of schedule is called a conventional fractionation schedule and uses external beam radiation, internal beam radiation or modern radiotherapy [4]. One cm thickness of Lipowitz alloy will effectively reduce an 18MeV electron beam by approximately 95%. The walls of the reservoir should be at least 0.5% thick to prevent backscatter of radiation [5]. The conventional technique, which is the facial moulage, is commonly used to fabricate these stents. Nowadays, computer-aided designing/computer-aided manufacturing (CAD/CAM) and rapid prototyping technologies have been used for the same [6].
Prosthesis in Radiotherapy
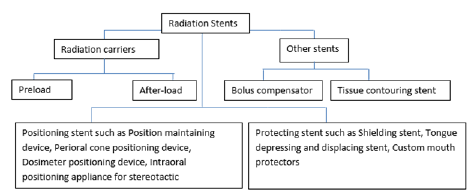
Many prostheses made by the dentist help the radiotherapist in treating patients with malignancies of oral and para oral tissues [7]. They can be divided into the following types [5]: (Figure 1)
Radiation carriers or surface applicators mostly use capsules, beads, tubes or needles made of a radioactive element such as radium 226, iridium192 or cesium132. They can carry the radiation sources close to the site of treatment (intracavitary) or directly into the tumor (interstitial). They are of two types; preloaded carriers and after loaded carriers [8]. A pre-loaded carrier incorporates the radioactive material like iridium seeds within a smaller diameter polyethylene tube which is then incorporated within the stent and Cerrobend shield is added. In an after-loaded carrier, the radioactive elements are placed after the carrier is in position, which reduces radiation exposure. This technique is used for both interstitial and intracavitary radiotherapy and is the preferred technique.
A Position maintaining stent displaces the movable tissues like the lips, tongue, cheeks and soft palate away from or towards the source of radiation [9]. A Perioral cone positioning stent holds the intraoral cone in a definite position and places the tongue away from the field of irradiation [10,11]. A Radiation measuring stent/ Dosimeter positioning stent contains lithium fluoride capsules that enable the radiotherapist to measure radiation received by tissues in contact with the capsule [5]. An Intraoral positioning appliance for stereotactic radiotherapy serves as an alternative to the conventional surgery for treatment of intracranial tumors [12] and delivers fractionated doses of radiation to the lesion from several different positions enabling the radiation oncologist to maximize the target dose while minimizing the dose to normal tissues [13]. A Shielding stent of a specific thickness of acrylic and containing lead or Cerrobend can be used to protect structures that are adjacent to the radiation therapy sites like the tongue shielding devices and lip shielding devices [10].
A custom mouth protector is a flexible smooth protector that protects painful edematous mucosal tissues from irritation by tooth surfaces and irritating foods [5]. Because of this reason, it is used mostly in sports-related activities to prevent injuries. A Tissue bolus compensator/Balloon bolus supporting stent helps in the treatment of superficial lesions of the face which have evident irregular contours. A tissue equivalent material, known as the bolus, is placed directly onto the irregularities that help in converting irregular tissue contours into flat surfaces, thereby, more accurately aid in the homogenous distribution of the radiation [14,15]. A Tissue recontouring stent serves to flatten the lip and ensures that its entire length lies in the same plane and ensures that a low dose of radiation is delivered at the corners of the mouth and high dose at the center.
Potential side effects of the radiation prostheses
In preload carrier, as the radioactive source is placed within the prosthesis before the carrier is inserted, it becomes mandatory for the dentist to deliver the prostheses urgently as the team members have a high chance of exposure to potentially hazardous radiations while performing the procedure [16]. Because of the stated problem, the preferred technique is the after load one in which the dentist provides hollow catheters in predetermined locations. Once the carrier is placed in the position, radioactive isotopes are allowed to enter into the hollow tubing for radiation therapy.
Lead cylinders have been used previously around the radiation prostheses to protect the surrounding normal tissues from irradiation effects. Lead’s high melting point, and potential toxicity are the reasons for its replacement by several alloys like Cerrobend that melts at lower temperatures [17].
Conclusion
It is thus recommended that a multidisciplinary approach be considered while treating a patient with head and neck cancer wherein a Surgeon, a Radiotherapist and a Prosthodontist must be on the team for a consultation before planning the treatment. These measures will help provide better treatment and improve the quality of life of the patient.
Conflict of Interest
The authors do not have any conflict of interest in the manuscript.
References
- Kanehira H, Shimizutani K, lnoue H (2005) Dental prostheses for patients after radiotherapy of the head and neck. J Osaka Dent Univ 39(1): 27-31.
- Beumer J, Curtis TA, Firtell DN (1979) Radiationtherapy of head and neck tumors: oral effects anddental manifestation. In maxillofacial Rehabilitation (Prosthodontic & Surgical Consideration). The CV Mosby Company Chp.3, 23.
- Walker C, Wadd NJ, Lucraft HH (1999) Novel solutions to the problems encountered in electron irradiation to the surface of the head. Br J Radiol 72(860): 787-791.
- (2016) Radiation Therapy.
- Ashish R Jain, T Janani, Suganya R (2016) Clinical Demonstration of Various Radiation Stents- An Overview. J Pharm Sci & Res 8(12): 1358-1366.
- Zemnick C, Woodhouse SA, Gewanter RM, Raphael M, Piro JD (2007) Rapid prototyping technique for creating a radiation shield. J Prosthet Dent 97(4): 236-241.
- Santiago A (1965) An intraoral stent for the direction of radiation beam therapy. J Prosthet Dent 15(5): 938-944.
- Mantri S, Bhasina S (2010) Preventive prosthodontics for head and neck radiotherapy. Journal of clinical and diagnostic research 4: 2958-2962.
- Santiago A (1965) Use of intraoral prosthesis in radiotherapy. Med Rec Ann 58: 3-11.
- Goswami R, Agarwal K, Gaba N (2013) Prosthetic Carriers for Radiation Therapy of Head and Neck. British Biomedical Bulletin 1(2): 136-146.
- Parel SM, Drane JB (1975) A modified intraoral prosthesis for directing a radiation beam. J Prosthet Dent 33(6): 666-671.
- Glenn E Minsley, Steven Rothenberg (1985) Use of the after loading technique for intraoral radiation carriers. Maxillofacial Prosthetics L Dental Implants 53(5): 676-678.
- Satish Gupta, Shailesh Jain (2015) Customized Radiation Prosthesis: A Preventive Approach for Head & Neck Radiotherapy. Indian Journal of Dental Sciences 2(7).
- Mantri SS, Bhasin A (2010) Preventive Prosthodontics for Head and Neck Radiotherapy. J Clin Diagn Res 4: 2958-2962.
- Brosky M, Lee C, Barlett T, Lo S (2000) Fabrication of radiation bolus prosthesis for the maxillectomy patient. J Prosthet Dent 83(1): 119-121.
- Derhei PM, Lim WC, Timmerman RD, Andres CJ (2003) Use of computed tomography for fabrication of a custom brachytherapy carrier: A clinical report. J Prosthet Dent 89(1): 15-18.
- Jayant Palaskar, Zankhana S Mody, Shreyas S Mohile, Jyoti H Wankhade, Sayali R Korde, et al. (2016) Different types of Radiation Prostheses to minimize radiation side-effects”, International Journal of Current Research 8(6): 33575-33578.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.