Case Report 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Cavernous Lymphangioma in the Mediastinum in an Adult Patient. Case Report
*Corresponding author: Gamboa Hoil Sergio Isidro, Department of Surgery, Oncology Hospital, National Medical Center Siglo XXI, Mexican Institute of Social Security, Mexico.
Received: September 27, 2019; Published: October 23, 2019
DOI: 10.34297/AJBSR.2019.05.000973
Abstract
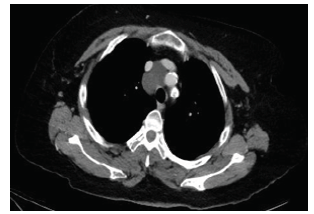
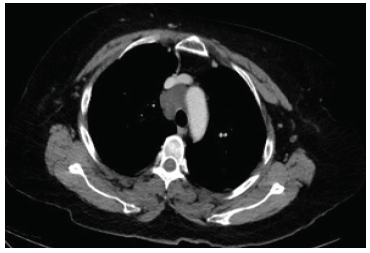
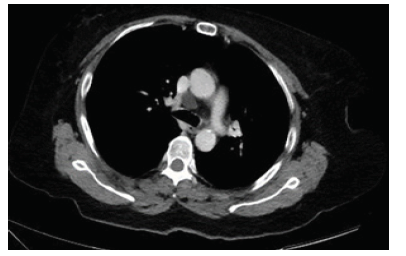
A 52-year-old woman presents thoracic intermittent pain, in computed tomography (CT), shows an oval image with a density of 20 UH. In the surgery, we found in medium mediastinum a tumor of 7 cm, lobulated, cystic aspect related in the anterior side with superior vena cava, external side vein with azigos vein, and internal side with Aorta. Report histopathology is cavernous lymphangioma. Cavernous lymphangioma is a congenital malformation, includes focal proliferations well differentiated of lymphatic tissue. Approximately 1% are confined to the thorax, most commonly located in the mediastinum, represent 0.7%-4.5% of all mediastinal tumors.
Keywords: Lymphangiomas; Cavernous Lymphangioma; Surgery.
Introduction
Lymphangioma was first described by Redenbacker in 1828 [1]. It is rare benign congenital malformations involving focal proliferations well-differentiated of lymphatic tissue [2]. Probably represent embryological remains of lymphatic ducts, which arose from portions of lymphatic sacs that were hijacked during development or could not connect to the efferent channels [3]. Approximately 1% of all lymphangiomas are confined to the thorax, most commonly located in the mediastinum, where represent 0.7%-4.5% of all mediastinal tumors. [2] We present the case of an adult woman with cavernous mediastinal lymphagioma.
Clinical Case
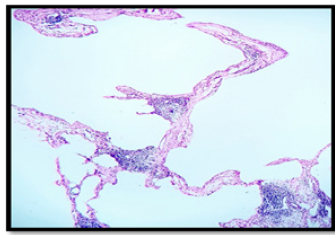
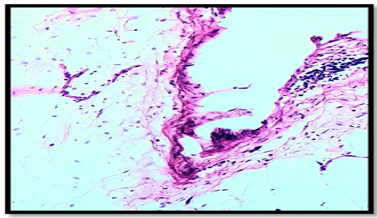
A 52-year-old woman with a history of diabetes mellitus, hypertension, heart failure functional class I, primary hypothyroidism, Cushing’s syndrome of pituitary origin, treated with bilateral adrenalectomy. During the follow-up of Cushing’s syndrome, presents intermittent painful, without dyspnea or weight loss. Computed tomography (CT), shows an oval image, lobulated contours, well delimited, homogeneous, with a density of 20 UH, which extends from the prevascular space to the upper and lower paratracheal of 4.1 x 3.2 x 5.7 cm. (Figure 1a, b, c ). After evaluation by the surgeon, surgery is decided. Performed posterolateral thoracotomy+ mediastinal tumor resection, we found in medium mediastinum a tumor of 7 cm, lobulated, cystic aspect related in the anterior side with superior vena cava, external side vein with azigos vein, and internal side with aorta. Report histopathology is cavernous lymphangioma (Figure 2a, b, c ).
Discussion
Charruau L, et al. in a series of 9 patients, described according to the locations in the mediastinum, 2 patients with lymphangioma in the anterior mediastinum, 4 patients in right paratracheal location, 1 patient in subcarinal location, 1 patients in aortopulmonary location and 1 patient with lymphangioma located below the left hilum with extension to the posterior mediastinum [4].
Teramoto, et al. reported mean age in 36.4 years, range of 20-57 years, with a slight predominance of women, [2] according to Park J et al, the size of the tumor varies of 1.7 to 12.0 cm, with a median of 6.1 cm and incidence of 1 x every 70,000 cases / year [1].
Patients may present asymptomatically, cough and dyspnea may be observed due to extrinsic compression of the respiratory tract; it can also be observed stridor, hemoptysis, Horner’s syndrome, dysphagia, superior vena cava syndrome, constrictive pericarditis, phrenic nerve paralysis, or symptoms related to a secondary lymphangioma infection [2,5].
Histologically, lymphangiomas are thin-walled unilocular or multilocular cystic tumors lined by endothelial cells that contain a light-yellow fluid [6]. They are subdivided into three types according to the size of the lymphatic channels they contain, cystic, capillary and cavernous. Cystic lymphangiomas are the most common, and the cavernous type is relatively rare [2]. Cavernous lymphangiomas present indiscrete margins and insinuate themselves into the surrounding structures [5]. Immunohistochemistry staining for CD31 confirms the diagnosis of mediastinal cystic tumors, as well as positive D2-40 staining for the endothelium of the lymphatic vessels and positive staining of the epithelium with cytokeratin AE1/3. The cavernous lymphangiomas have discrete amounts of loose connective tissue compared with the cystic lesions, which may be covered with thick adventitia. The connective tissue stromas consist of varying amounts of smooth muscle cells in the form of a spindle, bundles of collagen, fibroblasts and lymphocytes. The presence of benign lymphoid aggregates is useful in the identification of lymphangiomas. The cellular components are generally well differentiated and lack cytological atypia [5].
On chest radiographs, lymphangiomas are observed as welldefined and round masses; unilateral or bilateral pleural effusions may be present. Computed Tomography (CT) shows a smooth, lobulated mass that can wrap and / or displace adjacent mediastinal structures. They usually have a homogeneous attenuation like water, but it´s can also have a greater attenuation or a combination of liquid, solid and fat. It´s can be loculated or multiloculated. In magnetic resonance imaging (MRI), a heterogeneous signal intensity can be observed in T1, while in T2, show a high signal intensity [4,7].
Surgery is often required to confirm the diagnosis and prevent complications arising from compression in vital structures [2]. Okubo T, et al. and Oshikiri T, et al. reported a complete resection avoids recurrences after surgery [8,9].
Park J et al, observed recurrences occur up to 33%, with a mean until the recurrence of 3.6 years, but recurrences have been observed up to 10 years after surgery. The reported recurrence was local and all cases when the complete resection was not performed due to its proximity to vital structures [1].
With respect to survival among patients with lymphagioma and the expected survival for age and gender, no statistically significant difference was found (P = .13) [1].
Several alternative treatments have been tried, including chemotherapy, radiation therapy, sclerosing agents and laser therapy. The efficacy of these treatments is very variable in the incidental reports [3,10].
Interest conflict
The authors declare no conflict of interest
References
- Park J, Aubry M, Godfrey J, Midthun D (2006) Mediastinal lymphangioma: Mayo Clinic experience of 25 cases. Mayo Clin Proc 81(9): 1197-1203.
- Teramoto K, Suzumura Y (2008) Mediastinal cavernous lymphangioma in an adult. Gen Thorac Cardiovasc Surg 56(2): 88-90.
- Fokkema J, Paul M, Vrouenraets B (2014) Mediastinal lymphangioma in an adult. Ann R Coll Surg Engl 96(5): e24-e25.
- Charruau L, Parrens M, Jougon J, Montaudon M, Blachère H, et al. (2000) Mediastinal lymphangioma in adults: CT and MR imaging features. Eur Radiol 10(8): 1310-1314.
- Faul J, Berry G, Colby T, Ruoss S, Walter M, et al. (2000) Thoracic lymphangiomas, lymphangiectasis, lymphangiomatosis, and lymphatic dysplasia syndrome. Am J Respir Crit Care Med 161: 1037-1046.
- Mathew M, Dil S (2012) Adult lymphangioma-a rare entity: a report of two cases. Turk Patoloji Derg 28(1): 80-82.
- Jeung M, Gasser B, Gangi A, Bogorin A, Charneau D, et al. (2002) Imaging of cystic masses of the mediastinum. Radiographics. 22: S79-S93.
- Okubo T, Okayasu T, Osaka Y, Kajitani M, Hasegawa N, et al. (1992) Surgical analysis of mediastinal lymphangioma--analysis of 7 cases. Nihon Kyobu Geka Gakkai Zasshi 40(4): 583-586.
- Oshikiri T, Morikawa T, Jinushi E, Kawakami Y, Katoh H (2001) Five cases of the lymphangioma of the mediastinum in adult. Ann Thorac Cardiovasc Surg 7(2): 103-105.
- Suehisa H, Ueno T, Sawada S, Yamashita M, Teramoto N. et al. (2015) A Case of Mediastinal Cystic Lymphangioma. Acta Med Okayama 69(6): 361-363.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.