Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Nutritional Management of Immunological Diseases and Drug-Nutrient Interactions
*Corresponding author:Shewangzaw Addisu Mekuria, Assistant Professor, College of Veterinary Medicine and Animal Sciences, University of Gondar, P.O. Box 196 Gondar, Ethiopia.
Received: September 06, 2019;Published: September 19, 2019
DOI: 10.34297/AJBSR.2019.05.000906
Abstract
Background: Balanced nutrition, especially in terms of adequate vitamin, mineral and protein energy intake, enhances the resistance against infections. Nutrients can boost or depressed the immunity depending on the food nutrient and levels of intake. It can cause immunological disorder disease like Allergy, Asthma autoimmune diseases, HIV/AIDS, Rheumatoid Arthritis (RA), Celiac, Type I diabetics. A drug- nutrient interaction is the effect of medication on nutrients.
Methods: The information was collected from the google scholar and reviewed through Mendeley desktop with the objective of to review nutritional management of immunological diseases and drug-nutrient interactions.
Results: The interaction can be a positive and negative effect. One of the effects of this interaction were deficiency lead to vitamin or mineral deficiency. Medication can decrease appetite and sensory organs, nutrient absorption, nutrient production harmful bacteria and loss of nutrient.
Conclusion: Nutritional management of immunological disease affected people should be consider and an appropriate or alternative type of food. Drug-nutrient interactions can influence on food intake, nutrient digestion, absorption, and distribution, metabolism to active forms, function, catabolism, and excretion
Keywords: Drug Nutrient Interaction; Immunological Disease; Nutrition
Abbrevation: BHR: Bronchial Hyper-Responsiveness; DHAA: Dehydroascorbic Acid; GFD: Gluten-Free Diet; HAART: Highly Active Antiretroviral Therapy; PPIs: Proton Pump Inhibitors; PUFAs: Polyunsaturated Fatty Acids, RA: Rheumatoid Arthritis
Introduction
In man and other animals, nutrition and nutritional status can have profound effects on immune functions, resistance to infection and autoimmunity. Nutritional immunology altered supply of nutrients modifies immune response. It has become linked intimately with endeavors to improve the clinical patients who often require an exogenous supply of nutrients [1]. Depending on the nutrient and level of its intake nutrients enhance or depress immune function. Nutrients of protein-energy malnutrition and vitamin A deficiency are strongly associated with impaired immunity and infectious disease [2].
Immunological disorders are diseases or conditions caused by a dysfunction of the immune system include allergy, asthma autoimmune diseases, auto inflammatory syndromes, and immunological deficiency syndromes. The other issue under this paper is drug-nutrient interaction. A drug-nutrient interaction is the effect of a medication on food or a nutrient in food [3]. Medications interact with foods and nutrients in several ways. Medications can decrease appetite or change the way a nutrient is absorbed, metabolized, or excreted. Therefore, on the bases of the above definition, this paper aims to address the current research outputs of nutritional management of immunogenic disease and drug-nutrient interactions.
Methods
Information’s or data sources of nutritional management of immunogenic disease, and drug-nutrient interaction of the reviewed paper were first collected by using Harzing’s Publish or Perish google scholar software. After the collection of the required data sources the reviewed paper were analyzed by Mendeley Desktop.
Results and Discussion
Results
Nutritional Management of Immunogenic Disease: Nutritional management, also known as “food service management”, is the practice of providing nutritional options for individuals and groups with diet concerns through supervision of food services. The goal is to minimize the risk of complications, including infections during the treatment period, to attain and maintain normal nutritional status, to minimize metabolic disturbances during the treatment process. The most common immunogenic disease of the human being is Allergy (Asthma), Cilic disease, Rheumatoid arthritis, Diabetics Type I and HIV/AIDS
Drug-Nutrient Interactions: A drug-nutrient interaction is the effect of a medication on food or a nutrient in food. Medications interact with foods and nutrients in several ways. Medications can decrease appetite or change the way a nutrient is absorbed, metabolized, or excreted. A food-drug interaction is the effect of food or a nutrient in food on a medication [3]. Medications are used commonly to treat acute and chronic illness. Another definition of drug-nutrient interaction is that it is an interaction resulting from a physical, chemical, physiologic, or pathophysiologic relationship between a drug and a nutrient, multiple nutrients, food in general, or nutritional status [4]. Drugs can influence food intake, nutrient digestion, absorption, and distribution, metabolism to active forms, function, catabolism, and excretion
The interaction of drug-nutrient negative outcomes [1], including Death, Dehydration, Malnutrition, Decreased quality of life, Skin integrity deficits, Vitamin or mineral toxicity, or deficiency, Drug toxicity, or decreased efficiency of the drug, Elimination pattern changes (constipation or diarrhea, excessive or inadequate urine output), Change in PO intake patterns etc The long-term use of prescription and over the counter drugs can induce subclinical and clinically relevant micronutrient deficiencies, which may develop gradually over months or even years [5]. For individuals taking medications, drug-nutrient interactions may lead to vitamin or mineral deficiencies.
Discussion
Allergy: Asthma is a chronic inflammatory lung disease, associated with airway constriction, inflammation, bronchial hyper-responsiveness (BHR), as well as respiratory symptoms such as coughing, wheezing, dyspnoea and chest tightness [6]. It has been proposed that changing diet has contributed to the increase in asthma. According to the American dietary management of disease symposium which was cited by [7], Fish and fish oils are sources of long-chain omega-3 (n-3) PUFAs. These fatty acids act to oppose the actions of n-6 PUFAs, particularly about eicosanoid synthesis. Thus, n-3 PUFAs may protect against allergic sensitization and allergic manifestations. Dietary intake of saturated fats (butter and lard) has decreased and consumption of n-6 polyunsaturated fatty acids (PUFA) present in margarine. There was also a report on cow’s milk intake had a positive association with asthma [8]. The wide consumption of cow’s milk thus renders it an attractive strategy for prevention if the risk of infections were to be overcome
In addition to these, a different research study was reported on food allergy which shows that there was a causal link between increased intake of omega-6 (n-6) polyunsaturated fatty acids (PUFAs) and increased incidence of allergic disease has been suggested [9]. Thus, according to the author long-chain omega-3 (n- 3) PUFAs act to oppose the actions of n-6 PUFAs particularly about eicosanoid synthesis. Therefore, the recommended food sources for such allergies were fish and fish oils. There was also an agreement by [10] idea which was conducted on five epidemiological studies for a higher intake of fish lower risk of allergic disease in the offspring during infancy and childhood. However, according to the study of [11] intakes of omega-3 (n-3) PUFAs during pregnancy were associated with an increased risk of asthma in the offspring. [12] also reported for a person food allergy essential fatty acids, zinc, and vitamin D are likely to enhance the anti-inflammatory and antioxidative barrier and promote immunologic tolerance. Additionally, [13] also suggest that modulation of human breast milk composition has the potential for preventing allergic diseases (food Allergy, Asthma, and Eczema) in early life. Breastfeeding alters a child’s gut microbiome and subsequent immune development and influences the risk of respiratory infections through maternal antibody transfer.
Rheumatoid Arthritis (RA): Rheumatoid arthritis (RA) is a systemic, debilitating, chronic inflammatory autoimmune disorder affecting approximately 1% of the world population. Symptoms such as pain, joint stiffness, swelling, tenderness, and associated disability. A diet treatment studied and reported by [14] indicated a fasting of 7–10 days with partial nutrient intake of vegetable broth, herbal teas, parsley, garlic, and decoction of potatoes; juice extracts from carrots, beets, and celery; and a controlled daily energy intake followed by 1 year. The result shows a remarkable decrease in swollen and tender joints, pain, erythrocyte sedimentation rate (ESR), and C-reactive protein (CRP). According to the report of [15] evidence relating to other fatty acids, antioxidants, zinc, iron, folate, other B vitamins, calcium, vitamin D and fluoride are also considered. The present evidence suggests that RA patients should consume a balanced diet rich in long-chain n-3 PUFA and antioxidants.
Celiac: The coeliac disease also spelled celiac disease, is a long-term autoimmune disorder that primarily affects the small intestine. Coeliac disease is caused by a reaction to gluten, which is various proteins found in wheat and other grains such as barley and rye. According to the report of [16], the gluten-free diet (GFD) is a critical medical treatment for the millions of individuals worldwide. However, the gluten-free packaged foods have a more in fat and sugar-containing than their gluten-containing. Obesity, overweight, and new-onset insulin resistance and metabolic syndrome have been identified after initiation of a GFD [17].
Type I Diabetics: Type I diabetes mellitus develops because of autoimmune destruction of the insulin-producing B-cells of the pancreatic islets [18]. Carbohydrates are the main type of food that raises blood sugar. The starch, fruit and milk groups of the Food Group Pyramid for Diabetes are high in carbs. Foods in the Other Carbohydrates and Combination Food groups are also high in carbs. It is better to follow the Diabetes Food Pyramid:
A. Grains, Beans, and Starchy Vegetables (6 or more servings a day) Foods like bread, grains, beans, rice, pasta, and starchy vegetables are at the bottom of the pyramid because they should serve as the foundation of your diet. As a group, these foods are loaded with vitamins, minerals, fiber, and healthy carbohydrates. It is important, however, to eat foods with plenty of fiber. Choose whole-grain foods such as whole-grain bread or crackers, tortillas, bran cereal, brown rice, or beans. Use whole-wheat or other wholegrain flours in cooking and baking. Choose low-fat breads, such as bagels, tortillas, English muffins, and pita bread
B. Vegetables (3-5 servings a day) Choose fresh or frozen vegetables without added sauces, fats, or salt. You should opt for darker green and deep yellow vegetables, such as spinach, broccoli, romaine, carrots, and peppers.
C. Fruits (2-4 servings a day) Choose whole fruits more often than juices. Fruits have more fiber. Citrus fruits, such as oranges, grapefruits, and tangerines, are best. Drink fruit juices that do NOT have added sweeteners or syrups.
D. Milk (2-3 servings a day) Choose low-fat or nonfat milk or yogurt. Yogurt has natural sugar in it, but it can also contain added sugar or artificial sweeteners. Yogurt with artificial sweeteners has fewer calories than yogurt with added sugar.
E. Meat and Fish (2-3 servings a day) Eat fish and poultry more often. Remove the skin from chicken and turkey. Select lean cuts of beef, veal, pork, or wild game. Trim all visible fat from meat. Bake, roast, broil, grill, or boil instead of frying.
F. Fats, Alcohols, and Sweets In general, you should limit your intake of fatty foods, especially those high in saturated fat, such as hamburger, cheese, bacon, and butter. Limit the amount of drink alcohol with a meal. Sweets are high in fat and sugar, so keep portion sizes small. Other tips to avoid eating too many sweets.
HIV/AIDS: HIV/AIDS is a major global health problem and is currently the fourth leading cause of death in the world. It is an epidemic, severe and fatal disease. Nutritional management of people with HIV/AIDS has become increasingly complex since the introduction of new antiretroviral agents taken in combinations referred to as highly active antiretroviral therapy (HAART) [3]. The nutritional problems are significant and contribute to health and death in HIV+/AIDS patients. Serum antioxidant vitamins and minerals decrease while oxidative stress increases during AIDS progression.
The optimization of nutritional status, intervention with foods and supplements, including nutrients and other bioactive food components, are needed to maintain the immune system. According to the report of [19], probiotics or lactic acid bacteria and prebiotics are sometimes given on the presumed basis that they help maintain the integrity of mucosal surfaces, improve antibody responses and increase white blood cell production. Some general advice to help maintain weight and avoid loss of muscle mass (Food and Nutrition Technical Assistance [20]: Eat small amounts of low-fat food frequently to ensure better digestion and absorption of nutrients, Eat a variety of foods on a daily basis, Avoid alcohol, Avoid smoking, Eat more when recovering from an illness to make up lost weight
Drugs on Vitamins Vitamin B12: a. Proton Pump Inhibitors (PPIs) on Vitamin B12: Is a medication which is categorized Acid-Suppressing Drugs. The main action of PPIs is to reduce gastric acid production. Thus, decreased absorption of micronutrients that depend on low pH for uptake into intestinal cells may occur with PPI use [5].
Gastric acid is needed to remove B12 from dietary protein for intestinal absorption. The form of vitamin B12 in fortified foods and dietary supplements does not require gastric acid and proteolysis to liberate it from protein binding [5]. There were conflict research outputs were reported between PPIs and Vitamin B12. According to the findings of [21] a research conducted on older adults use of PPIs for 12 months were measuring serum B12 has an association of an increased risk of B12 deficiency. However, [22] were reported research on elderly patients on PPI therapy >3 years found no significant difference in serum B12 levels compared to non-PPI users, after adjusting for age, C-reactive protein levels, and H. pylori infection. Therefore, according to the review of [5] age is another potential risk factor for B12 deficiency with PPI use. The previously described cross-sectional studies that showed a higher risk of B12 deficiency (as measured by serum B12 levels) with long-term PPI use were performed in adults >60 years. [22], also reported on the effects of omeprazole on B12 status are due solely to impaired gastric acid secretion. Its significantly lower levels of serum B12 after one year of omeprazole use than patients without the mutation. Therefore, according to the research report of [23], drinking acidic fruit juice concurrently with B12 may improve absorption in PPI users.
Vitamin C:
a. Protein Pump Inhibitors on Vitamin C: Vitamin C is highly concentrated in gastric juice, where it is predominantly found in its biologically active antioxidant form, ascorbic acid (AA). In addition to acting as an antioxidant, AA in gastric juice functions to eliminate potentially carcinogenic nitrites from saliva [5]. In this process, AA is converted into its inactive form, dehydroascorbic acid (DHAA), which cannot be absorbed in the intestine [24]. However, on the report [25] it may be converted back to AA through a pH-dependent process for reabsorption. According to the findings of [25] on the volunteers of with and without H. pylori infection treatment with 40 mg/d omeprazole for four weeks significantly reduced the proportion of AA to total vitamin C concentrations in gastric juice from all volunteers and increased intragastric pH
b. Aspirin on Vitamin C: Aspirin also interferes with absorption of vitamin C, and regular use of aspirin can deplete your gastrointestinal lining of vitamin C. There is limited research has conducted the interaction of aspirin and vitamin C absorption. According to the findings of [26] in the human study, the concentrations of vitamin C in plasma, leucocytes, and urine were found to be markedly elevated at various intervals following administration of a single oral dose of 500 mg of the vitamin. The vitamin C-associated increases, however, appeared to be blocked when the vitamin was given simultaneously with aspirin (900 mg). These results suggest that aspirin may impede gastrointestinal absorption of vitamin C.
Drugs on Minerals
Iron:
a. PPIs on Iron: Non-heme iron is the predominant form of iron found in plant foods and must be reduced before absorption in the small intestine. Therefore, PPI use may affect its absorption. According to the report of [27], omeprazole-induced achlorhydria may impair the response to iron supplementation in patients who were previously iron-deficient. In summary, there is some evidence to indicate PPI use may negatively impact iron absorption.
b. Aspirin on Iron: It is well established that aspirin use can cause gastric mucosal damage, gastric ulcers, and increase the risk of gastrointestinal bleeding, even at low doses [5]. Aspirin use is associated with lower serum ferritin (SF). They were reported that a man who took >7 aspirins/wk had a significantly lower (by 25%) geometric mean SF than did nonusers, who took <1 aspirin/ wk (71 compared with 95 μg/L, respectively; P for trend = 0.004). This effect of aspirin on SF was more marked in diseased subjects than in healthy subjects (mean SF was 50% lower compared with 21% lower, respectively). Therefore, it is possible a long-term aspirin regimen may decrease iron stores, increasing the risk for iron-deficiency anemia. According to the report of [28], surprising studies show that there are a few dietary supplements that can help protect the stomach from aspirin side effects. One of them is probably sitting on your shelf right now: vitamin C. This everyday vitamin acts as an antioxidant in the stomach to decrease aspirininduced stomach damage.
Calcium
a. PPIs on Calcium: Calcium absorption in the small intestine is influenced by gastric Ph. Therefore, similar concerns have been raised regarding PPI use, calcium absorption, and bone health in chronic PPI users [29]. However, different scholars wrote on the effect of PPIs on the absorption of Ca and it was controversial. b. Anti-Hypertensives: Diuretics on Calcium: Diuretic agents have variable effects on calcium excretion as studied in vivo and isolated kidneys and nephron segments [29]. Generally, by increasing sodium and water excretion, diuretics will cause a concomitant increase in calcium excretion
Magnesium
a. PPIs on Magnesium: Hypomagnesaemia and associated hypocalcemia and hypoparathyroidism have been increasingly recognized as rare long-term side-effects of proton pump inhibitors (PPIs) [30]. According to their study on four patients treated by PPIs, series developed hypomagnesemia, which responded to withdrawal of therapy and initiation of Mg replacement. So, long term use of PPIs has an association of hypomagnesemia
b. Anti-Hypertensives: Diuretics on Magnesium: Some clinicians contend that hypomagnesemia is a common problem in patients receiving diuretic therapy and that routine serum magnesium determinations may be indicated in such patients. According to the findings of [31] for determined serum magnesium (Mg++) levels in 354 patients with uncomplicated hypertension. No significant difference was observed in the mean Mg++ between the 245 diuretic-treated patients and the 109 patients not receiving diuretics. When analyzed by type of diuretic, there were statistically significant differences in the mean serum Mg++ concentrations between those receiving thiazides, those receiving no diuretics, and those receiving triamterene-containing diuretics. These absolute differences, however, were clinically quite small, and hypomagnesemia was uncommon
Zinc
a. PPIs on Zinc: According to the study of [4] the effects of administering the acid secretion inhibitor cimetidine (1 g/day for 3 days) and to evaluate the influence of HCl gastric secretion on zinc absorption in physiological conditions. Zinc absorption was reduced after cimetidine administration. The author also confirmed by comparing ranitidine and Cimetidine on gastric acidity of man by monitoring 60-min intervals throughout the test via a nasogastric tube. Gastric acid was reduced after ranitidine (300 mg), but not after cimetidine (500 mg) administration, suggesting that gastric acid secretion plays a role in the regulation of zinc absorption in man.
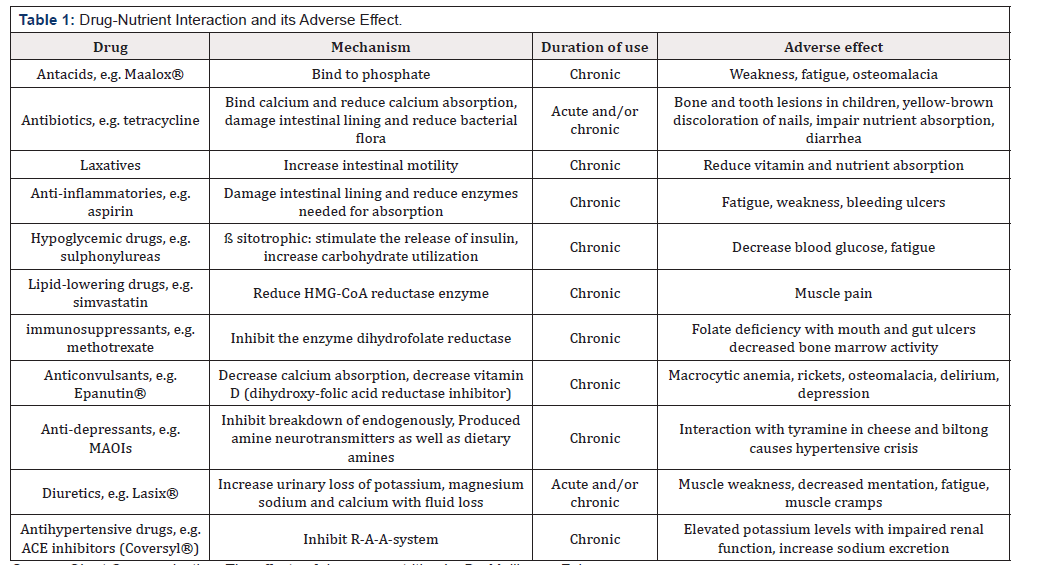
b. Anti-Hypertensives: Diuretics on Zinc: There was a research report output on ACE inhibitors, thiazide diuretics, beta-blockers, or ARB drugs of which five included a control group Studies used urinary zinc excretion, plasma zinc levels or erythrocyte zinc as key measures of zinc status [34]. Therefore, the available evidence suggests that the use of thiazide diuretics have the potential to reduce zinc levels in hypertensive patients (Table 1) [33,34].
Source- Short Communication: The effects of drugs on nutrition by Dr. Mollie van Zyl
Generally, Principles of Drug-Nutrient Interaction A. Medications can decrease appetite or cause nausea, vomiting, an unpleasant taste, or dry mouth. This can affect nutritional health by causing poor food intakes such as Appetite suppressants, several cancer medications, and treatment. B. Medications can decrease nutrient absorption. Example: Laxatives can decrease the absorption of many vitamins and minerals. Laxatives cause food to move rapidly through the body causing poor nutrient absorption. Some anticonvulsants can decrease folate absorption.
C. Medications can slow down nutrient production. Example: Vitamin K is produced by bacteria in the intestines. Antibiotics kill harmful bacteria, but they can also kill helpful bacteria, including bacteria that produce vitamin K in the intestine. D. Medications can interfere with the body’s ability to metabolize nutrients. Example: Some anticonvulsants alter the activity of liver enzymes, causing increase metabolism of folate, vitamin D and vitamin K.
E. Medications can increase the loss of a nutrient. Example: Diuretics remove excess fluid from the body. Some diuretics may also increase the loss of potassium along with fluids. Potassium is very important in the proper functioning of the heart and other muscles.
Conclusion
Generally, the dietitian should be considering or recommend an alternative type (Variety) of food for those who are immunogenic disease affected peoples. Drug-nutrient interactions had a relationship between a drug and a nutrient, and typically involve multiple factors. It can influence on food intake, nutrient digestion, absorption, and distribution, metabolism to active forms, function, catabolism, and excretion. So, we should provide the type of nutrients of food for the specific type of drug. Based on this review still, there is a gap and further research on: - The consequence and relationship of nutrients and immunogenic disease, Antioxidant food with the interaction of immunogenic disease and Drug interaction on major nutrients.
Acknowledgement
The authors express his sincere gratitude to University of Gondar, Ethiopia, Jomo Kenyatta University and RUFORUM/DAAD
References
- Saeed F, Nadeem M, Ahmed RS, Tahir M, Arshad MS, et al. (2016) Studying the impact of nutritional immunology underlying the modulation of immune responses by nutritional compounds- a review. 0105
- Harbige LS (2017) Nutrition and Immunity with Emphasis on Infection and Autoimmune Disease. Nutr Health 10(4): 285-312
- Hermann J, Ld RD (2017) Drug Nutrient Interactions. Division of Agricultural Sciences and Natural Resources Oklahoma State University
- Sturniolo GC, Montino MC, Rossetto L, Martin A, D’Inca R, et al. (2013) Inhibition of gastric acid secretion reduces zinc absorption in man. J Am Coll Nutr 10(4): 372-375
- Emily S Mohn, Hua J Kern, Edward Saltzman SHM, DLM (2018) Evidence of Drug - Nutrient Interactions with Chronic Use of Commonly Prescribed Medications: An Update. Pharmaceutics 10(1): E36
- Banafshe H, Bronwyn SB, Wark P, Wood LG (2017) Effects of Fruit and Vegetable Consumption on Risk of Asthma, Wheezing and Immune Responses: A Systematic Review and Meta-Analysis. Nutrients 9(4): 341
- Devereux G (2018) Symposium on ‘Dietary management of disease’ Session 1: Allergic disease Nutrition as a potential determinant of asthma Proceedings of the Nutrition Society. Proc Nutr Soc 69(1): 1-10
- Brick T, Ege M, Boeren S, Vervoort J, Id KH, et al. (2017) Effect of Processing Intensity on Immunologically Active Bovine Milk Serum Proteins. Nutrients 9(9): E963
- Miles EA (2017) Can Early Omega-3 Fatty Acid Exposure Reduce Risk of Childhood Allergic Disease? Nutrition 9(784): 1-16.
- Lefkothea S, Kremmyda M, Vlachava PS, Elizabeth A Miles, PCC (2011) Atopy Risk in Infants and Children in Relation to Early Exposure to Fish, Oily Fish, or Long-Chain Omega-3 Fatty Acids_ A Systematic Review _ Springer for Research & Development. Clinic Rev Allerg Immunol 41(36): 36-66.
- Lumia M, Luukkainen P, Tapanainen H, Kaila M, Erkkola M, et al. (2011) Allergic Diseases and Asthma in Pregnancy-World Allergy Organization. Pediatery Allergy Immune 22(8): 827-835.
- Mazzocchi A, Venter C, Maslin K, Agostoni C (2017) The Role of Nutritional Aspects in Food Allergy: Prevention and Management. Nutrients 9(8): 1-12
- Munblit D, Peroni DG, Boix-amor A, Hsu PS, Land B, et al. (2017) Human Milk and Allergic Diseases: An Unsolved Puzzle. Nutrients 9(8): E894.
- Michalsen A, Riegert M, Lüdtke R, Bäcker M, Langhorst J, et al. (2005) BMC Complementary and Mediterranean diet or extended fasting’ s influence on changing the intestinal microflora, immunoglobulin A secretion and clinical outcome in patients with rheumatoid arthritis and fibromyalgia: an observational study. 9: 1-9.
- Rennie KL, Hughes J, Lang R, Jebb SA (2003) Nutritional management of rheumatoid arthritis: a review of the evidence. J Hum Nutr Diet 16(2): 97-109
- Reilly NR (2016) The Gluten-Free Diet: Recognizing Fact, Fiction, and Fad. The Journal of Pediatrics 1-5.
- Tortora R, Capone P, De Stefano G, Imperatore N, Gerbino N DS, et al. (2015) Metabolic syndrome in patients with coeliac disease on a gluten- free diet. Aliment Pharmacol Ther 41(4):352-359
- Hertzelc Gerstein (1997) Type 1 Diabetes Nutrition » UF Diabetes Institute. Gerstein 17(1): 13-19.
- Suttajit M (2007) Advances in nutrition support for quality of life in HIV+_AIDS. Asia Pac J Clin Nutr 16(1): 318-322.
- Fanta (2001) HIV/AIDS: A Guide for Nutrition, Care and Support July 2001
- Dharmarajan TS, Kanagala MR, Murakonda P, Lebelt AS, Norkus E (2008) Do acid-lowering agents affect vitamin b12 status in older adults? J Am Med Dir Assoc 9(3): 162-167.
- Den Elzen WPJ, Groeneveld Y, de Ruijter W, Souverijn JHM, le Cessie S, et al. (2008) Long-term use of proton pump inhibitors and vitamin B12 status in elderly individuals. Aliment Pharmacol Ther 27(6): 491-497.
- Saltzman J, Kemp J, Golner B, Pedrosa M, Dallal G, et al. (1996) Effect of hypochlorhydria due to omeprazole treatment or atrophic gastritis on protein-bound vitamin B12 absorption. J Am Coll Nutr 13(6): 584-591.
- Samaras D, Samaras N, Lang PO, Genton L, Frangos E, et al. (2013) Effects of widely used drugs on micronutrients: A story rarely told. Nutrition 29(4): 605-610.
- McColl KEL (2009) Effect of proton pump inhibitors on vitamins and iron. American Journal of Gastroenterology 104(2): S5-S9.
- Basu T (1982) Vitamin C-aspirin interactions. Int J Vitam Nutr Res 23: 89-90
- Sharma VR, Brannon MA, Carloss E (2004) Effect of omeprazole on oral iron replacement in patients with iron deficiency anemia. South Med J 97: 887-889.
- Leo Galland (2015) Aspirin and Vitamin C Together at Last.
- Stier CT, IH (1986) Renal calcium metabolism and diuretics. Annu Rev Pharmacol Toxicol 26: 101-126.
- Toh JW, Ong E, Wilson R (2015) Hypomagnesaemia associated with longterm use of proton pump inhibitors. Gastroenterol Rep 3(3): 243-253
- Kurt Kroenke, David R Wood, James F Hanley (1987) The Value of Serum Magnesium Determination in Hypertensive Patients Receiving Diuretics- JAMA Internal Medicine-JAMA Network. Arch Intern Med 147(9): 1553-1556.
- Braun LA, RF (2013) Pharmaco‐nutrient interactions-a systematic review of zinc and antihypertensive therapy. International Wiley Online Library 67(8): 717-725.
- Batterham M, Brown D, Garsia R (2001) Nutritional management of HIV/AIDS in the era of highly active antiretroviral therapy: a review. 58(4): 211-223.
- Sipponen P, Härkönen M (2010) Hypochlorhydric stomach: A risk condition for calcium malabsorption and osteoporosis? Scand J Gastroenterol 45(2): 133-138.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.