Review Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Pediatric Nursing Triage in Mass Gathering: Education and Training Issues
*Corresponding author: Farrag S, Faulty of Nursing, Mansoura University, Egypt.
Received: September 10, 2019;Published: September 20, 2019
DOI: 10.34297/AJBSR.2019.05.000908
Abstract
Deaths of children could occur during mass gathering due to various reasons. Many of these deaths could be prevented if very sick children were identified and appropriate treatment started immediately upon their arrival at the health facility. This study investigates standardized role of the pediatric nurse in Emergency Triage, and the real situation occurring in Makkah local governmental hospitals, where nurses can hardly participate in the assessment, or decision making, and how the guidelines are used in the process.
Significance of the study: Researchers have recently found that nurses reported limited knowledge and awareness of the wider emergency and disaster preparedness plans. This clarifies the research gap for pediatric nurses.
Aims of the study: (1) is to review all the available studies in order to come up with a clear standardized role of the pediatric nurse in Emergency Triage. (2) to describe the requirements needed by the newly graduated nurses in order to be categorized by Health Authorities as an Emergency Triage Pediatric Nurse. (3) to recommend the integration of Triage competencies in BSC nursing curriculum.
Setting: The study was conducted at the Faculty of Nursing, Umm Al Qura University, Saudi Arabia. Methods: A review of the literature on mass gatherings and triage systems, was conducted.
Four databases were utilized: (1) OVID (2) PubMed, (3) Cochrane Collection Plus, and (4) Lippincott. The search terms: Triage, Pre-hospital triage, Field triage, Triage nurse, Nursing curriculum, Pediatric nurse, Emergency room clinical competencies.
Results: Differences in the application of pediatric triage across local and international hospitals in Mass-Gathering events, are discussed. The lack of standardized role of pediatric nurses in emergency triage is demonstrated both on national and international levels.
Conclusion: Pediatric nurses should have a standardized role in emergency triage.
Recommendations: Pediatric triage in emergency settings must be integrated in BSC nursing curriculum.
Keywords: Triage; Pre-hospital triage; Field triage; Triage nurse; Nursing curriculum; Pediatric nurse; Emergency room clinical competencies
Introduction
Deaths of children in hospital often occur within the first 24 h of admission. Many of these deaths could be prevented if very sick children were identified and appropriate treatment started immediately upon their arrival at the health facility. This can be facilitated by rapid triage for all children presenting to hospital in order to determine whether any emergency or priority signs are present and providing appropriate emergency treatment. WHO therefore published guidelines and training materials for pediatric emergency triage, assessment and treatment (ETAT) [1]. WHO pediatric ETAT guidelines aim to identify children presenting with airway obstruction and other breathing problems, circulatory impairment or shock, severely altered CNS function (coma or convulsive seizures) or severe dehydration, because it is these children who require urgent appropriate care to prevent death [1].
In 2013, [2] WHO guideline development scoping group reviewed the pediatric ETAT guidelines and identified areas of care and specific recommendations that should be updated considering the new evidence and international consensus [2]. Three priorities for the care of sick infants and children were identified: detection of hypoxemia and use of oxygen therapy, fluid management of infants and children presenting with impaired circulation and management of seizures. This guideline is intended for use in low-resource settings to provide clinical guidance to these health workers on managing infants and children presenting with signs of severe illness [2]. In 2003, the USA adopted and designed the emergency severity index (ESI). All are 5 category scales. The triage categorization level procedures depend on the patients’ complaints and the vital signs as well as the expertise of the triage person(nurse/physician/others). It requires education and training.
Methods
Articles were reviewed by two team members, and relevant articles were obtained and reviewed by the team. Articles were selected from peer-reviewed journals; focused on the role of the nurse in pediatric triage (hospital and pre-hospital), the required clinical competencies, the expected number of years of experiences both in ambulatory care and ER too, the hospital policy regarding nursing role, the Ministry of Health as a governing body for qualified health professionals, and the nursing curriculum in the Faculties of Nursing in the Middle-Eastern Region. The aim is to encourage policy makers and Ministry of Education in collaboration with Ministry of Health, to make the case for the inclusion of training on triage in nursing education programs
Concept of Triage
‘‘Triage’’ is a useful tool used in emergency departments (EDs) to prioritize the care of patients. Through a methodical process of different sequential steps, the triage nurse assigns a color code which goes from red critical patient with immediate access to medical examination to a white code that represents no urgency. Clinical studies have shown that the incorrect assessment at triage represents one of the major errors in EDs and the patients can be victims of errors during the process of care, especially in complex systems such as EDs [3].
The triage recommended in the guidelines defines the priority to receive treatment using four color codes in the form of: Red (very critical, highest priority); Yellow (average critical, medium priority); Green (low critical, low priority, treatment can be delayed); and White (non-critical, urgent intervention is not required) [3]. Triage is defined as prioritizing or sorting the patients for the care and treatment, it is the process of determining the priority of patients’ treatments based on the severity of their condition. The term comes from the French verb trier, meaning to separate, sift or select. Triage may result in determining the order and priority of emergency treatment, the order and priority of emergency transport, or the transport destination for the patient. Triage may also be used for patients arriving at the emergency department or telephoning medical advice systems. the concept of triage as it occurs in medical emergencies, including the prehospital setting, disasters, and emergency room treatment [4]. The goals of Triage, as set forth by the Canadian Association Of Emergency Physicians (CAEP), the National Emergency Nurses Affiliation of Canada (NENA) are: (1) to rapidly identify patients with urgent, life threatening conditions (2) to determine the most appropriate treatment area for patients presenting to the ED (3) to decrease congestion in emergency treatment areas; to provide ongoing assessment of patients (4) to provide information to patients and families regarding services, expected care, and waiting times, and (5) to contribute information that helps to define departmental acuity [5].
What is a Triage Nurse?
Ebrahimi M et al. [6] concluded that Triage nursing as a relatively new role for nurses is a challenging role in a dynamic environment which needs significant development to be practiced. Prioritizing is defined as the pivotal role for triage nurse. Comprehensive educational programs and developmental research are required to support diagnostic and therapeutic interventions in triage practice by nurses. Moreover, triage nurses must be aware of alternative health care facilities, she must have a minimum degree of BS in nursing and must have a minimum 2-year experience in ED. Also, triage nurses must have a minimum 40-hour educational courses annually
A Triage Nurse is a registered nurse positioned in an emergency room (ER) or facility; responsible for assessing patients and determining their level of need for medical assistance. The criteria used to evaluate a patient include the type of injury or illness, its severity, symptoms, patient explanation of emergency, and vital signs. A Triage Nurse is typically the first point of clinical contact for patients visiting an ER. A nurse who is trained in triage is trained to quickly assess and sort patients so that they can get the proper attention and care [7-16]. The Emergency Nurses Association (ENA) has comprehensively indicated several educational programs (CPR, ALS) in addition to other triage educational programs. Furthermore, interpersonal qualifications including interpersonal, interdisciplinary, critical thinking, and communication skills as well as accurate decision making have been stated by several emergency associations. However, triage nurses are required to perform prioritizing of the patient care, take educational programs, and provide a safe environment as well as interpersonal qualifications needed to fulfill this role [17-20].
Knight A [21] confirmed that the role of the pediatric triage nurse is to have thorough knowledge of up to date practices in caring for the child, and to accurately assess and manage the child. Also, nurses triaging the unwell child should include evidencebased decisions in applying a triage category guideline, effective care including accurate and informed education of parents. Every nurse working on triage should maintain current knowledge and have continuous education concerning the child and the unwell child to promote best patient outcomes and maintain best practice standards. As stated in the emergency triage education kit: “The triage nurse makes urgency decisions and employs locally based policies and procedures to expedite care for all patients,”. Infants and small children differ from adults both psychologically and physiologically implicating challenging levels of assessment for the triage nurse. Initial and continuous assessment of the child is imperative to achieve best patient outcomes and reduce the risk of inaccurate triage assessments, and education of the parents is a role of the triage nurse that promotes comfort and security in the level of care being provided [22].
Role of Triage Nurse
According to Sinclair [10], the basic job description for triage nurse is the same for any registered nurse, plus at least 2 years of critical care experience in a large ICU setting. The role requires identification of nurses who possess the following qualities: a) Competency for working on several different units b) A capacity to work independently c) Goal oriented d) Self- directed e) Able to identify and set priorities f) Assertive with a positive attitude g) Able to work well with the professional staff
Aacharya et al. [23] illustrated that, the nurse must be able to calmly and capably communicate with a patient in need, ask appropriate questions, make good decisions quickly and focus in situations that might be highly stressful. Communication skills are essential, because triage nurses often must explain things to patients and their families as well as delegate certain tasks to other health professionals. A triage nurse is an important part of an emergency care team, working to ensure that patients who need treatment right away are prioritized properly. It is the job of a triage nurse to competently assess patients in emergency care. These may be patients suffering illness or patients who have been involved in accidents or other traumatic events. Since many patients can come through the doors of an emergency room, it is important that a trained and skilled nurse be able to decide who needs care most urgently. Some patients may be able to be treated quickly, while other patients may need to go to other parts of the hospital in order to have other services [24-28].
Delphi method was used to develop a role description of triage nurse relying on the emergency medicine experts. Based on Delphi method, Triage nurse is responsible for patients status until the first physician visit, manage ethical conflict in triage decisions, manage aggressive patients effectively, perform the first assessment in the ED, estimate life-threatening risk of chief complaints, prioritize patients based on assessing respirations, pulse rate, blood pressure, temperature, O2 saturation, and other diagnostic measures, follow organization’s guidelines during decision making [25]. Triage nurses are responsible for facilities of triage room and she are not permitted to leave the triage room. Triage nurses must document triage assignments and report daily and monthly statistics of triage. Diagnostic and therapeutic related interventions must be performed by triage nurses [11]. In case of doubt, triage nurses must consult with attending physician or head nurse, also in case of doubt, triage nurses must assign patient to the higher level of acuity. Triage nurses must reconsider their decisions if requested from medical directors. Triage nurses must explain waiting time to the first visit, explain necessary information relating to the patient condition, as well as explain necessary information relating to alternative facilities for care and treatment [9].
All triage is done by registered nurses (RNs), but the Emergency Nurses Association recommends that a nurse have more training and skills than just basic nursing. Some of the recommended components of that training includes CPR and ALS courses. Another important course they recommend is the Emergency Nurse Pediatric course, which trains nurses to work triage in disaster situations that involve children. Trauma nursing and geriatric emergency nursing courses are also recommended so nurses can be trained to handle a variety of patients in situations related to trauma and emergency. There may be other important courses for nurses preparing to work in triage, but these are considered some of the standard ones. Nurses in this area generally also work toward certifications as either a Certified Emergency Nurse (CEN) or a Certified Pediatric Emergency Nurse (CPEN) [29]. A Mirhaghi et al. [7] reported that responsibilities of a triage nurse include; Perform patient assessment, reassess patients who are waiting, initiate emergency treatment if necessary, manage and communicate with patients in waiting room, provide education to patients and families when necessary, sort patients into priority groups according to guidelines, transport patients to appropriate treatment areas, communicate status of patients to doctors and nurses, and triage nurses must also be able to multitask and make decisions when information is limited.
Pre-hospital and Field Triage During Mass-casualty Incidents and Disasters / Pre-hospital Care System and Emergency Medical Services (EMS)
Pre-hospital care also known as the post-crash response consists of the urgent medical care provided to patients at the scene of injury, within the ambulance or other transporting vehicle until patients are transported to the emergency department (ED) of a hospital. Post-crash response in particular starts from extracting victims from vehicles or in vicinity of the accident. Pre-hospital care is a series of interventions that start at the incident scene and end at the hospital. It is a part of a larger system, which is known as trauma system [30].
Pre-hospital care provides an urgent care that requires timely appropriate medical attention to save lives or minimize permanent disabilities. Improvement in patient care outcomes is associated with improvements in pre-hospital care system. The World Health Organization (WHO) encouraged countries in its 2011 global plan for road safety to implement five pillars: 1) road safety management 2) safer roads and mobility 3) safer vehicles 4) safer road users and 5) pre-hospital or post-crash response [31]. Pre-hospital care is a remote critical care triage process, where Emergency Medical Services (EMS) and care are received before reaching the hospital. However, two EMS models are followed in the world. One, known as Franco-German model, brings the hospital to the patient, where most of the patients are treated at the site of incident. While the other model, Anglo-American, brings the patient to the hospital, where patients are transported to the hospital emergency departments as promptly as possible. The former is based on “delay and treat” philosophy whereas the latter is a “load and go” [32]. Although both are considered successful EMS models, outcomes cannot be easily compared given the fundamental difference in their operational methods.
The primary aim of EMS is to prevent unnecessary mortality and long-term morbidity by providing timely critical medical care to acutely sick patients. The role of emergency medical providers is very crucial. It affects patient’s journey from the point of impact to hospital discharge. Therefore, EMS providers are always under the pressure to develop and maintain skills of quick and effective decision making with limited information [33]. The American College of Emergency Physicians and ENA published task-force recommendations (originally approved in 2003 and revised in 2010) to implement a “reliable, valid five-level triage scale such as the Emergency Severity Index (ESI)” [34]. Other examples of 5-level triage scores include the Canadian Triage and Acuity Scale, the Manchester Triage Scale, and the Australasian (National) Triage Scale. These indices are algorithmic and consider whether the patient is in extremis, the clinical context of presentation, the resources available, and vital signs. The triage scales have been applied successfully to adults and children and are appropriate tools to apply to a broad population who present to the emergency department with a variety of signs and symptoms [35].
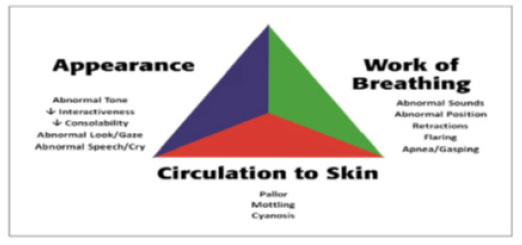
According to the study of Timothy Horeczko et al. [36], who stressed that The Pediatric Assessment Triangle (PAT) is a rapid evaluation tool that establishes a child’s clinical status and his or her category of illness to direct initial management priorities. Recently the PAT has been incorporated widely into the pediatric resuscitation curriculum. Emergency nurses can rely on the PAT as an objective early warning of children in or at high risk for clinical deterioration. It is especially helpful in cases when history and physical examination are limited. Furthermore, the PAT serves as a common vocabulary between health-care providers [37]. The Pediatric Assessment Triangle (PAT) generates a rapid, global assessment using only visual and auditory clues; it requires no equipment and takes seconds to perform. The PAT was designed to enable the provider to articulate formally a general impression of the child, establish the severity of the presentation and category of pathophysiology, and determine the type and urgency of intervention. Using the PAT, the provider makes observations of 3 components: appearance, work of breathing, and circulation to the skin (Figure 1) [38].
Nurses’ Involvement Decision Making
The decision-making process is commonly termed triage and has been described as the sorting of medical conditions into different categories to achieve a true priority of care [12]. There are several factors that support the involvement of nurses in CPR decision making. As a result of lengthy stays, nurses spend a lot of time with many long- term care patients and could be expected to have a good understanding of their values and beliefs. Nurses are usually the first responders during an in-hospital cardiac arrest and must either initiate CPR or withhold it. In order to fulfill their role as patient advocates, nurses need to be informed about decisions that affect their patients. Although nurses are infrequently consulted before the CPR decision making process, several studies have reported that they desire greater involvement and they believe they can offer a unique and worthwhile perspective [39].
The Resuscitation Council (UK) recommends that doctors, nurses, medical students and student nurses should be trained to use automatic external defibrillators (AEDs) to facilitate early defibrillation, and that AEDs should be available to all non- critical ward areas. The nursing position is reinforced by the chief nurse (UK) who, as part of the “National Health Service plan” to raise standards, recommends nurse defibrillation as a basic rather than an extended role. Nurses are key health care professionals for using AEDs in hospitals and for teaching other first responders--inside and outside hospitals--how to use AEDs. Although the use of AEDs by nursing staff has been suggested and implemented in many hospitals, studies assessing the results of this practice are limited with small sample size [40]. For nurses to initiate defibrillation there is clearly a need for a widespread change in philosophy as well as equipment. Simply introducing AEDs may not be enough to improve survival. First, nurses must accept defibrillation as a primary rather than extended role. The concept of nurse-initiated defibrillation is supported by many nurses. Combining AED training with annual BLS training may facilitate the acceptance of defibrillation as a nursing role and assist in its wider dissemination [41].
Researchers in the USA in the early 1980s found that triage was associated with a wide range of patient handling activities during disasters. If, however, triage was the prioritization of victims based upon assessment of need, the evidence suggested this rarely occurred. Certainly, in the UK there is an expectation that triage should be carried out at the scene of a major incident, and both the NHS Executive in England and Ambulance Service Association refer to on scene triage, yet neither document outlines what exactly is meant by triage. This can only lead to confusion—who should be performing triage, what form of triage should be used, triage for treatment (triage sieve) or for transportation (triage sort), should other models of triage be used, what skills should prehospital emergency care providers be taught? It is entirely possible that each provider on scene is using a different approach to triage without universal understanding [12].
Hajj Mass Gathering
Hajj is a unique gathering with Mecca and Kaaba being spiritually important to many faiths across the globe, especially Muslims. This is because of the proclamation of the prophet’s father, Ibrahaam, when he called all mankind to perform Hajj. That is why all Muslims on Earth feel that they must visit Mecca and Kaaba on a specific date and time, and that is the reason this small location hosts one of the largest human gatherings in the world [15]. The World Health Organization (WHO) defines mass gatherings as “events attended by a sufficient number of people to strain the planning and response resources of a community, state or nation. Mass gatherings can have good and bad long-term effects on the health sectors of host countries. As the largest annual mass gathering in the world, the hajj or pilgrimage to Mecca overburdens Saudi Arabia’s health system because 2 to 3 million Muslim pilgrims from more than 180 countries converge on the country’s holiest sites [8].
Ministry of Health in Saudi Arabia
Infection was a frequent feature of the Hajj especially with poor pre-Hajj Health care from Pilgrims came from low-income countries, crowded accommodations. Poor hygiene, unknown medical background, Extreme heat, poor prepared stored food and inadequate pre-Hajj vaccination are leading to many of infectious diseases like respiratory/airborne diseases, Meningitis, food/water borne diseases and blood borne diseases. Apart from vaccination in a pandemic situation, the effectiveness of yearly influenza vaccination for Hajj pilgrims is questionable because of differences in the viral strains used in vaccines in the northern and southern hemispheres [42].
The Saudi Minster of Health recognized the threat early and instituted a variety of infectious control measures, including screening, Monitoring port of entry and isolation for suspected cases, surveillance for infectious diseases epidemiology, and computer-based information systems, laboratory testing, infection control; and provide proper treatment [26]. Saudi recommendation to all pilgrims to wear surgical facemask when in crowds, hands hygiene and to be vaccinated against seasonal influenza [27]. Saudi Ministry of Health reported the preventive measures to control the infectious diseases as follow updated annual vaccination, enforcement of regulations about food and water security, regulation of head shaving and sterilized razors, Pilgrims awareness for hands hygiene, adequate hydration, facemask use, Sunscreen, Insect repellents, food and water and personal hygiene, avoid severe crowds. Initiate self-treatment as needed, continue usual medications, reporting illness and recommendations about respiratory hygiene. These improvements have taken place at the same time as important changes to infrastructure, including accommodation for pilgrims to reduce overcrowding and risk of spread of infection [19].
Triage During Mass Gatherings
Triage is a complex process and is one means for determining which patients most need access to limited resources. Triage has been studied extensively, particularly in relation to triage in overcrowded emergency departments. The need for an effective triage and acuity scoring system for use during mass gatherings is clear, as these events not only create multiple patient encounters, but also have the potential to become mass-casualty incidents. Furthermore, triage during a large-scale disaster or mass-casualty incident requires that multiple, local agencies work together, necessitating a common language for triage and acuity scoring [43]. Scant research has been done to develop and test an effective triage approach for use in mass-gathering and mass-participation events, although there is a growing body of knowledge regarding the health needs of persons attending large events. Existing triage and acuity scoring systems are suboptimal for this unique population, as these events can involve high patient presentation rates (PPR) and, occasionally, critically ill patients. Mass-gathering events are dangerous; a higher incidence of injury occurs than would be expected from general population statistics [43].
Telephone Triage
Practices have been encouraged to develop flexible models of access tailored to local needs. Telephone triage, in which a patient requesting a face-to-face appointment is, in the first instance, offered a call back from a doctor or nurse, is increasingly being adopted to manage demand. During the telephone call, the need for an appointment can be assessed and the most appropriate management plan agreed, including a face-to-face follow-up consultation if appropriate. Because a proportion of patients do not immediately require any further contact extending beyond the telephone call, this system would appear to be more efficient than the usual care arrangement in which face-to-face appointments are provided without triage [44].
Study of Tim A. Holt et al. concluded that telephone triage is not associated with a reduction in overall clinician contact time during the index day. Introducing telephone triage in primary care requires careful consideration of the organizational structure and culture, staff skills and experience, perceived need and anticipated outcomes, staffing issues, and the geographical location and primary care setting in which triage might be introduced [45]. Murdoch et al. [46] concluded that staff experiences and perceptions of telephone triage are shaped by the way practices communicate with staff, prepare for and sustain the changes required to implement triage effectively, as well as by existing practice culture, and staff and patient behavior arising in response to the changes made. Telephone triage reconfigures the function, skills and identities of staff according to how the activities of their everyday working practice shift as a result of its introduction. Staff resources need to be appropriately allocated in order to ensure staff are not overburdened, and appointment sessions need to be organized in line with triage sessions to ensure appointments are not wasted and that patients are not being inappropriately triaged into emergency slots [47].
Conclusion
1. Triage nursing as a relatively new role for nurses needs significant development to be practiced. Comprehensive educational programs and developmental research are required to support diagnostic and therapeutic interventions in triage practice by nurses. 2. Pediatric Assessment Triangle (PAT) as evaluation tool has been incorporated widely into the pediatric resuscitation curriculum. 3. Triage related interventions still need extensive development to be reliable enough to practice by triage nurses. 4. A nurse without specific training in triage and inexperienced in critical care was identified as the ‘‘root cause’’ of the sentinel event. To make improvements we planned a triage training course (for newly employed nurses and a refresher course for existing staff) and created a team of dedicated triage nurses. 5. Telephone triage, in which a patient requesting a faceto- face appointment is, in the first instance, offered a call back from a doctor or nurse, is increasingly being adopted to manage demand.
6. Due to the annual Hajj pilgrimage, Emergency Medicine training in Saudi Arabia emphasizes mass gathering casualty care, disaster preparedness and ability to cope with multicultural people with no background medical knowledge. Emergency Medicine training programs include a National Hajj Preparation course and mandatory Hajj rotation during the residency program to prepare for this real-world challenge [18]. 7. Nurses have insufficient knowledge about disaster preparedness due to a lack of acceptance of core competencies and the absence of disaster preparedness in nursing curricula. 8. The recommendation that education in disaster preparedness, response and management must be included and further developed in basic nursing programs as well as in all postgraduate nursing programs.
9. The nursing education community has agreed that the existing curricula are too focused on content and do not teach the most vital nursing skills of critical thinking, clinical reasoning, and decision-making [48]. In fact, the National League for Nursing in the United States mandates that critical thinking skills must be included in nursing programs in order to gain accreditation. 10. language barriers are a major issue for triage nurses, especially in terms of comprehending the subtle nuances of critical messages. In effort to reduce such misunderstandings as well as to establish better clinician-patient communication for such hospitals, it would be wise to offer classes on basic foreign language skills for health professionals [49].
11. Inaccurate decisions and systemic inefficiency of triage nurses, despite their degree of experience, can result in patients being under-triaged or over-triaged. 12. Specific to pediatric emergency departments, most of the patient data is gathered from the parents. For this reason, nurses in pediatric triage training should be taught specific skills and techniques in information gathering when dealing with the parents. 13. Emergency departments typically have structured triage guidelines for health care providers. Such guidelines aid in determining which patients must be evaluated promptly and which may wait safely, and aid in determining anticipated use of resources [50].
References
- WHO (2005) Emergency triage assessment and treatment (ETAT). Switzerland
- WHO (2013) Guideline: updates on the management of severe acute malnutrition in infants and children. Switzerland
- De Luca C, Francia S, Gabriele G, Guasticchi Eilgruppo, Triage Modello Lazio (2012) Come implementare un modello di Triage di pronto soccorso. L’esperienzadellaregione Lazio Ann Ig 20: 431-439.
- Husted, Ernie (2011) Principles of Triage During A Mass Casualty Incident: MASS, START, Id-me, RPM
- Husted, Ernie (2011) Principles of Triage During A Mass Casualty Incident: MASS, START, Id-me, RPM
- Ebrahimi M, Mirhaghi A, Mazlom R, Heydari A, Nassehi A, et al. (2016) The Role Descriptions of Triage Nurse in Emergency Department: A Delphi Study. Hindawi Publishing Corporation Scientifica 2016: 1-6.
- A Mirhaghi, H Kooshiar, H Esmaeili, M Ebrahimi (2015) Outcomes for emergency severity index triage implementation in the emergency department. Journal of Clinical and Diagnostic Research 9(4): OC04-OC07
- Al Tawfiq JA, Memish ZA (2012) Mass gatherings and infectious diseases: prevention, detection, and control. Infect Dis Clin North Am 26(3): 725-737
- D Bahena, C Andreoni (2013) Provider in triage: is this a place for nurse practitioners? Advanced Emergency Nursing Journal 35(4): 332-343.
- Sinclair T (2006) The role of the Rapid Response Nurse: hospital-wide and in trauma resuscitations. J Trauma Nurs 13(4): 175-177
- R Boulkedid, H Abdoul, M Loustau, O Sibony, C Alberti (2011) Using and reporting the Delphi method for selecting healthcare quality indicators: a systematic review. PLoS ONE 6(6): e20476
- Kennedy K, Aghababian RV, Gans L (1996) Triage: techniques and applications in decisionmaking. Ann Emerg Med 28(2): 136-144.
- Gilboy N, Tanabe P, Travers D, Rosenau A (2001) Emergency Severity Index (ESI): A triage tool for emergency department care, Version 4. Implementation Handbook. 2012 edition. Rockville (MD): AHRQ Publication p. 1-91.
- A Mirhaghi, H Kooshiar, H Esmaeili, M Ebrahimi (2015) Outcomes for emergency severity index triage implementation in the emergency department. Journal of Clinical and Diagnostic Research 9(4): OC04-OC07
- Asaad Shujaaa, Sameer Alhamidb (2015) Health response to Hajj mass gathering from emergency perspective, narrative review. Turk J Emerg Med 15(4): 172-176.
- BH Rowe, C Villa Roel, X Guo, Bullard MJ, Ospina M, et al., (2011) The role of triage nurse ordering on mitigating overcrowding in emergency departments: a systematic review. Academic Emergency Medicine 18(12): 1349-1357
- ((2011) The Emergncy Nurses Association, Triage Qualifications: Position Statement, ENA. Des Plaines, Ill, USA
- Hsieh YH, Ngai KM, Burkle FM, Hsu EB (2009) Epidemiological characteristics of human stampedes. Disaster Med Public Health Prep 3(4): 217-223.
- Habib AG, Abdulmumini M, Dalhat MM, Hamza M, Iliyasu G (2010) Anti- retroviral therapy among HIV infected travelers to Hajj pilgrimage. J Travel Med 17(3): 176-181
- (2011) The College of Emergency Medicine Clinical Effectiveness Committee, Emergency Nurse Consultant Association, Faculty of Emergency Nursing, Royal College of Nursing Emergency Care Association, Triage Position Statement, CEM, London, UK.
- Knight A (2015) Triage nurse’s assessment of a child with a fever. Clinical update, Anmforgu 22(10).
- Dixon G, Deehan D, Dickson R, Miller, Pegnam Mason H (2006) Clinical and consumer guidelines related to the management of childhood fever: An Emergency Triage Education Kit 2009. Commonwealth of Australia
- Aacharya RP, Gastmans C, Denier Y (2011) Emergency department triage: an ethical analysis. BMC Emergency Medicine. 11: 16
- F Hasson, S Keeney, H Mc Kenna (2000) Research guidelines for the Delphi survey technique. Journal of Advanced Nursing 32(4):1008-1015.
- S Keeney, F Hasson, HP Mc Kenna (2001) A critical review of the Delphi technique as a research methodology for nursing,” International Journal of Nursing Studies 38(2): 195-200
- Ebrahim SH, Memish ZA, Uyeki TM, Khoja TA, Marano N, et al. (2009) Public health. Pandemic H1N1 and the 2009 Hajj. Science 326(5955): 938-940.
- (2010) Health conditions for travellers to Saudi Arabia for the pilgrimage to Mecca (Hajj) Wkly Epidemiol Rec 85: 425-428.
- Visser L, Montejano A, Grossman V (2015) Fast Facts for the Triage Nurse. Springer Publishers, New York p. 1-32.
- J Considine, E Lucas, R Payne, M Kropman, HE Stergiou, et al. (2012) Analysis of three advanced practice roles in emergency nursing. Australasian Emergency Nursing Journal 15(4): 219-228.
- Organization WH (2010) Eastern Mediterranean status report on road safety: call for action. p. 1-100.
- Mazur S, D Ellis (2014) Right people, right time: Prehospital and Retrieval Medicine. Emergency Medicine Australasia 26(5): 423-425.
- Al Shaqsi S (2010) Models of International Emergency Medical Service (EMS) Systems. Oman Med J 25(4): 320-323.
- Krug E (2012) Decade of action for road safety 2011-2020. Injury 43(1): 6-7.
- (2010) American College of Emergency Physicians. Emergency Nurses Association. Joint Statement by the American College of Emergency Physicians (ACEP) and the Emergency Nurses Association (ENA): Triage Scale Standardization. American College of Emergency Physicians, USA
- Hohenhaus SM, Travers D, Mecham N (2008) Pediatric triage: a review of emergency education literature. J Emerg Nurs 34: 309-313
- Timothy Horeczko, Brianna Enriquez, Nancy E Mc Grath, Marianne Gausche Hill, Roger J Lewis (2013) The Pediatric Assessment Triangle: Accuracy of Its Application by Nurses in the Triage of ChildrenJ Emerg Nurs 39(2): 182-189.
- Moll H (2010) Challenges in the validation of triage systems at emergency departments. J Clin Epidemiol 63(4): 384-388.
- Van Veen M, Steyerberg EW, Ruige M, van Meurs AH, Roukema J, et al. (2008) Manchester triage system in paediatric emergency care: prospective observational study. BMJ p. 337.
- Nolan JP, Soar J, Zideman DA, Biarent D, Bossaert LL, et al. (2010) European Resuscitation Council Guidelines for Resuscitation 2010 Section 1. Executive summary. Resuscitation 81(10): 1219-1276.
- Xanthos T, Ekmektzoglou K, Bassiakou E, Koudouna E, Barouxis D, et al. (2009) Nurses are more efficient than doctors in teaching basic life support and automated external defibrillators in nurses. Nurse Educ Today 29(2): 224-231.
- Kenward G, Castle N, Hodgetts T (2002) Should ward nurses be using automatic external defibrillators as first responders to improve the outcome from cardiac arrest? A systematic review of the primary research. Resuscitation 52(1): 31-37.
- Memish ZA, Charrel RN, Zaki AM, Fagbo SF (2010) Alkhurma haemorrhagic fevera viral haemorrhagic disease unique to the Arabian Peninsula. Int J Antimicrob Agents 36(Suppl 1): S53-S57.
- Turris SA, Lund A (2012) Triage during mass gatherings. Prehosp Disaster Med 27(6): 531-535.
- Royal College of General Practitioners (2013) The 2022 GP: A vision for general practice in the future NHS. RCGP, London.
- Tim A Holt, Emily Fletcher, Fiona Warren, Suzanne Richards, Chris Salisbury, et al. (2016) Telephone triage systems in UK general practice: analysis of consultation duration during the index day in a pragmatic randomized controlled trial. British Journal of General Practice 66(644): e214-e218.
- Murdoch J, Varley A, Fletcher E, Britten N, Richards D, et al. (2015) Implementing telephone triage in general practice: a process evaluation of a cluster randomized controlled trial. BMC Family Practice 16: 47.
- Murdoch J, Barnes R, Pooler J, Lattimer V, Fletcher E, Campbell JL (2014) Question design in nurse-led and GP-led telephone triage for same-day appointment requests: a comparative investigation. BMJ Open 4(3): e004515.
- Candela L, Dalley K, Benzel Lindley J (2006) A case for learning-centered curricula. Journal of Nursing Education 45(2): 59-66.
- Hampers LC, Mc Nulty JE (2002) Professional interpreters and bilingual physicians in a pediatric emergency department: Effect on resource utilization. Archives of Pediatrics & Adolescent Medicine 156(11): 1108- 1113.
- Campbell JL, Fletcher E, Britten N, Green C, Holt TA, Lattimer V, et al. (2015) The clinical effectiveness and cost-effectiveness of telephone triage of patients requesting same day consultations in general practice: study protocol for a cluster randomized controlled trial comparing nurse-led and GP-led management systems (the ESTEEM trial). Health Technol Assess 19(13): 1-212.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.