Research Article 
 Creative Commons, CC-BY
Creative Commons, CC-BY
Clinical Pharmacists in Chronic care [Part 1]
*Corresponding author: Abdul Kader Mohiuddin, Department of chemistry, University Memorial Trust, Tejgaon, Dhaka, Bangladesh.
Received: September 27, 2019; Published: November 01, 2019
DOI: 10.34297/AJBSR.2019.06.000991
Abstract
Pharmacy practice has changed substantially in recent years. The professionals could contribute directly to patient care in order to reduce morbimortality related to medication use, promoting health and preventing diseases. Healthcare organizations worldwide are under substantial pressure from increasing patient demand. Unfortunately, a cure is not always possible particularly in this era of chronic diseases, and the role of physicians has become limited to controlling and palliating symptoms. The increasing population of patients with long-term conditions are associated with high levels of morbidity, healthcare costs and GP workloads. Clinical pharmacy took over an aspect of medical care that had been partially abandoned by physicians. Overburdened by patient loads and the explosion of new drugs, physicians turned to pharmacists more and more for drug information, especially within institutional settings. Once relegated to counting and pouring, pharmacists headed institutional reviews of drug utilization and served as consultants to all types of health-care facilities. In addition, when clinical pharmacists are active members of the care team, they enhance efficiency by: Providing critical input on medication use and dosing. Working with patients to solve problems with their medications and improve adherence.
Keywords: Chronic care; Pharmacy intervention; Diabetes care; CVD prevention; Inflammatory bowel disease
Abbrevation: American Association of Colleges of Pharmacy (AACP); Accreditation Council for Pharmacy Education (ACPE); International Diabetes Federation (IDF); Hemoglobin A1c (HbA1c); Ischemic Heart Disease (IHD); Myocardial Infarction (MI); Coronary Heart Disease (CHD); Disability- Adjusted Life Year (DALY); Quality of Life (QoL); Drug Related Problems (DRPs); Inflammatory bowel disease (IBD); Hormone replacement therapy (HRT); Bone-Mineral Density (BMD); Chronic obstructive pulmonary disease (COPD); LDL cholesterol (LDL-C); Gastroesophageal Reflux Disease (GERD)
Background
Clinical pharmacology is a professional discipline that combines basic pharmacology and clinical medicine. A clinical pharmacist offers invaluable support in the development of a final prescription with better patient management and enhanced safety [1]. Its development began in the early 1950s, primarily as a result of the efforts of Harry Gold. Pharmacist rounding with inpatient hospital services has been traced to the University of Kentucky in 1957 [1,2]. Drug therapy was becoming much more complex. Graham Calder pioneered a new role for pharmacists on hospital wards in Aberdeen [3]. The role of clinical pharmacists underwent important changes from the 1960s through 1990s as their participation in direct patient care increased. In the early 1970s, federal funding assisted with greatly expanding clinical pharmacy faculty in Colleges of Pharmacy [4]. Pharmacy education debated where clinical pharmacy fit within pharmacy training. The AACP spearheaded an effort to examine this issue. Till then, two full generations of pharmacists have been educated and trained after the general adoption of the aims of clinical pharmacy [4,5]. ACPE has revised the standards for colleges and schools of pharmacy several times since 2000. ACPE Standards 2016 go into effect July 1, 2016 Figure 1.

Figure 1:Clinical pharmacy offers chronic care services like asthma, diabetes, nutritional supplement counseling, smoking cessation, weight reduction, geriatric care, hyperlipidemia, hypertension, naturopathy and wound care. The integration of clinical pharmacists into primary care clinics could have positive effects on the clinical outcomes of patients in glycemic control, blood pressure, lipid profile, in accordance with current guidelines.
To some extent, pharmacy took over an aspect of medical care that had been partially abandoned by physicians [6]. Overburdened by patient loads and the explosion of new drugs, physicians turned to pharmacists more and more for drug information, especially within institutional settings. A clinical pharmacist often has a somewhat different approach to the use of drugs and may give valuable supplementary information about for example interactions, during the physician’s decision-making process concerning potential changes of and the follow-up of the medication [7,8]. The concept of pharmaceutical care emphasizes the pharmacists’ responsibility to pursue the best possible patient outcomes of medication therapy [9]. They possess in-depth knowledge of medications that is integrated with a foundational understanding of the biomedical, pharmaceutical, socio-behavioral, and clinical sciences [10]. To accomplish wanted therapeutic goals, the clinical pharmacist applies proof based therapeutic guidelines, developing sciences, rising advancements, and important lawful, moral, social, social, financial, and proficient standards [11-13]. In understanding, clinical pharmacists accept accountability and responsibility for overseeing medication therapy in direct patient consideration settings, in the case of rehearsing freely or in meeting or joint effort with other healthcare professionals [14,15].
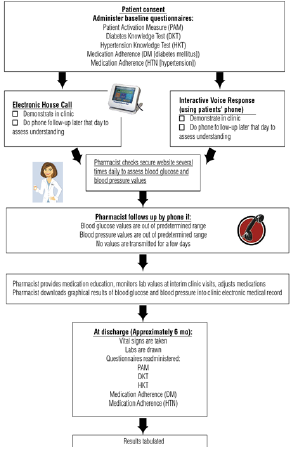
Figure 2:Telemonitoring model for providing clinical pharmacy services to patients with diabetes [62].
Their functions encompass comprehensive medication management (i.e., prescribing, monitoring, and adjustment of medications), nonpharmacologic guidance, and coordination of care. Interdisciplinary collaboration allows pharmacists opportunities to provide direct patient care or consultations by telecommunication in many different clinical environments, including disease management, primary care, or specialty care [16-19]. Pharmacists may manage chronic or acute illnesses associated with endocrine, cardiovascular, respiratory, gastrointestinal, or other systems [20]. Clinical pharmacist researchers generate, disseminate, and apply new knowledge that contributes to improved health and quality of life [21-24]. Inside the arrangement of healthcare, clinical pharmacists are specialists in the therapeutic utilization of medications. They routinely give medication therapy assessments and suggestions to patients and healthcare professionals [25,26]. Clinical pharmacists are an essential wellspring of logically legitimate data and counsel about the sheltered, proper, and financially savvy utilization of medications [27,28]. They get restorative and medication history, check medication blunders including prescription, dispensing and administration mistakes, distinguish drug interactions, screen ADR, propose individualization of measurement routine, give patient counseling, and so forth [29-35]. They also provide information about the use of drugs and medical devices like inhaler, insulin pen, eye drops, nasal sprays, etc. [36]. Participation of a clinical pharmacist in ward/ICU rounds and clinical CVD Preventions helps to identify, prevent or reduce drug interaction and ADR [29], [37-39] Figure 2.
Introduction
Population aging has increased the burden of chronic diseases globally. There are both ethical and reasonable goals to address health inequity issues identified with chronic disease management for people with social multifaceted nature, existing programs regularly don’t fittingly address the necessities of these people. This prompts low degrees of support in programs, imperfect chronic disease management, and higher healthcare usage [40]. Unlike acute conditions, chronic diseases require consistent care and management outside of the healthcare setting, in the community or primary care setting, in terms of medication, lifestyle management, and health behavior modification [41-45]. It is typically a multicomponent intervention that includes medication therapy review, patient medication education, medication monitoring, immunizations, disease self-care and support, and/or prescribing authority. Patients who take multiple medications due to chronic disease have a high risk of drug duplication, interaction, or adverse side effects, which could result in extended hospital stays and higher costs [46]. To increase the safety and effectiveness of treatment, these patients must have specific needs met, with regards to appropriate medication use [47]. Studies have shown that integrating pharmacists into ambulatory clinics can improve chronic disease management and optimal use of medications [48]. Besides, pharmacist contribution in patient care may decrease unseemly medication use, explicitly in the old. A study in Canada saw the extent of patients accepting an improper medication drop essentially after medication audit and enhancement by a group that incorporated a pharmacist [49]. Contrasted with regular care, pharmacist-drove care was related with comparable frequencies or paces of office, earnest care or ED visits, and hospitalizations and medication adherence, expanded the number or portion of medications got and improved study-selected glycemic, circulatory strain, and lipid objective achievement [50]. Another recent study shows telehealth-based chronic disease management program including clinical pharmacy specialists imparted statistically significant improvements in diabetes and hypertension outcomes along with clinically significant improvements in the areas of lipid management and tobacco cessation [51].
Diabetes Care
As the seventh-leading cause of death in the US, diabetes can lead to various health complications such as blindness, kidney disease, amputations, and heart disease. The worldwide existing prevalence of DM is about 425 million people, of whom 279 million are in urban areas and 146 million are in rural zones [52]. The IDF estimates that by 2040, one in 10 adults (642 million) will have diabetes. Around 50% (212.4 million) of patients are unaware of their diabetes. More than 12% of total global health expenditure goes to diabetes, according to IDF [53]. Annual worldwide economic cost of diabetic care was calculated at $727 billion in year 2017 which is predicted to be $776 billion for year 2045 respectively [54]. Currently, more than 230 million Asian individuals are living with diabetes, accounting for approximately 55% of the world’s diabetic population. China and India collectively are home of nearly 110 million diabetic patients [55]. It is a risk factor for CVD and has been related with 2-4-fold higher mortality [56] and another study says that half of all diabetic demise was expected to CVD [57]. The quantity of deaths brought about by diabetes in the age scope of 60-99 years in 2017 was 3,200,000 [58]. About portion of diabetes-related mortality (48%) happens in people more youthful than 60 years and it keeps on diminishing future by 6-8 years in people analyzed at 50 years old years [59]. Over 35% patients didn’t get any diabetes education, while 30% diabetic patients were compliant with drug regimens and the non-compliance was higher among the lower socioeconomic groups [60].
Pharmacist may provide a face-to-face counseling regarding knowledge on diabetes, self-monitoring of blood glucose, regular checkup of systolic blood pressure, body weight, and serum cholesterol levels. The pharmacist may also counsel regarding non-pharmacological management strategies such as diet control, exercise therapy, and early identification of symptoms of hypoglycemia (blurred vision, rapid heartbeat, sweating, fatigue, headache, dizziness, trouble thinking, seizures, and coma) and its management. In a satisfaction survey of 24 providers or clinical pharmacists, nearly 90% had favorable responses toward the protocol and its effect on access to and quality of care [61]. Management of DM remains a significant challenge in the US, as estimates indicate that greater than 40% of diabetes patients are uncontrolled with a HbA1c. Diabetic patients who received care from the collaborative team, including a clinical pharmacist, had improvement in most key indicators of diabetes like HbA1c, in both high and low-income countries and in both urban and rural areas [62-71]. Emphasizing medication adherence, particularly for patients with longer duration of diabetes and those with multiple comorbid diseases should be strongly considered in future diabetes management programs implemented to improve glycemic control in patients with type 2 diabetes [72]. A mobile phone text message can serve as a simple and cost-effective option in improving medication adherence and clinical outcomes by providing information between clinic visits has been reported [73,74]. A report from the National Diabetes Commission suggested that an inappropriate attitude of health care professionals toward diabetes could lead to poor patient outcomes [75]. In educational program, a clinical or community pharmacist can improve adherence by giving medication consultation administration, making an individualized patient timetable on administration times and dosage of every medication, instructing the patient on the significance of medication adherence dietary adherence and exercise on better glycemic control, offering guidance on the best way to diminish adverse effects of medications, and furthermore by instructing how to take medications in the holy month of Ramadan or different religious fasting, and how to utilize pill boxes and diary logs to decrease absent mindedness. Writing demonstrates various interventional studies including pharmacistbased educational intercessions, indicating clinically noteworthy enhancements in the clinical results of the diabetes patients [76].
CVD Prevention
Hypertension is the single most important risk factor for CVD and a key driver of global disease burden [77]. It is a major risk factor for CHD, stroke, retinopathies, and renal dysfunction. 18 million people die each year from CVDs, an estimated 31% of all deaths worldwide [78]. Of these deaths, 85% are due to MI and stroke [79]. CVD is currently the leading cause of morbidity and mortality and over 80% occur in LMICs [80]. Nearly 50% patients with chest pain related to exercise have obstructive coronary artery disease [81]. Coronary artery spasm plays an important role in the pathogenesis of IHD, including angina pectoris, MI, and sudden death, occurring most often from midnight to early morning [82].
A study of 1,015 patients with stable coronary artery disease showed a 4.4-fold increase in the risk of stroke and a 3.8-fold increase in the risk of death among patients who self-reported as nonadherent [83]. IHD has topped the list of causes of years of life lost for more than a decade, highlighting the shift in the global burden of disease from communicable to chronic disease. Risk factors for CVD, including raised blood pressure, hypercholesterolemia and high BMI, are among the most important contributors to DALYs [84]. CVD claimed death of some 900,000 death in US in 2016 [85]. BP is yet uncontrolled in half of the US population with hypertension. Moreover, BP can remain ineffectively controlled regardless of up to six doctor visits for each year [86].
Crosswise over South Asia, in general hypertension prevalence is assessed to be 27%. Prospective Urban Rural Epidemiology study has demonstrated over half are ignorant of it and up to 80% of hypertensive patients have low adherence to medication. Uncontrolled BP was discovered over half in Bangladesh, 70% in Pakistan and practically 60% in Sri Lanka [87]. The goals of treatment of hypertension are to restrict target organ damage, in this manner decreasing the horribleness and mortality related with the disease [88]. Numerous factors including financial status, conviction about medications, comorbidity, accessibility of medications, access to healthcare, level of health proficiency, number of medications, duration of therapy, age, gender, culture, educational status, and learning of the disease and treatment have been related with the pace of adherence. Absence of medication accessibility, low degree of mindfulness about the disease and treatment, failure to manage the cost of prescriptions, question in western drug, and more trust on traditional and spiritual healers are exceptionally normal in the rural population [89].
Non-drug therapies have been shown to lower BP, enhance antihypertensive drug efficacy, and decrease cardiovascular risk. All patients with hypertension and those in the prehypertensive category should be advised to make life-style modifications in addition to any pharmacologic treatment that they receive [90]. Surprisingly, 60%- 80% of the population around the world (according to WHO) are partially or fully dependent upon herbal drugs for primary healthcare [91]. Interactions of certain ingredients in supplements with other anti-hypertensive and cardiovascular arrangements are well-reported [92]. Green tea demonstrated 85% abatement in plasma concentration of nadolol, for instance [93]. The pharmacist may assume a significant job in primary and secondary prevention of cardiovascular diseases, chiefly through patient education and counseling, drug safety management, medication audit (survey of both drug-food and drug-drug cooperation), monitoring and reconciliation, discovery and control of explicit cardiovascular risk factors (e.g., circulatory strain, blood glucose, serum lipids) and clinical outcomes [94].
Pharmacist intervention can increase patients’ knowledge about their condition in a way that positively modifies their beliefs about medicines, increased medication intensification without significant change in medication adherence, modify factors affecting adherence, improve adherence and patient QoL by reducing BP levels in patients treated with antihypertensive agents, increased referral acceptance [86], [95-99]. Interventions that were most effective included combinations of more convenient care, information, reminders, self-monitoring, reinforcement, counseling, family therapy, psychological therapy, crisis intervention, manual telephone follow-up, and supportive care [83]. Weight loss has been noted to modify risk factors via improving insulin sensitivity, reducing inflammation, decreasing blood pressure and modifying the lipid profile [100]. It is astonishing that 7-28% of patients with coronary heart disease still smoke, but around half of smokers are planning to quit [101]. The World Bank proposes that around 180 million tobacco related deaths could be forestalled among now and 2050 if grown-up tobacco utilization diminished by half by 2020 [102].
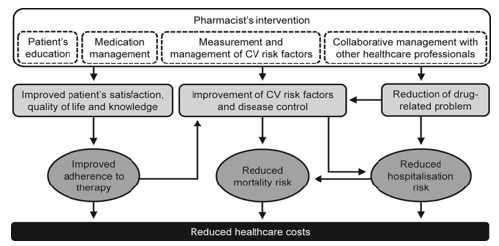
Figure 3: Effects of pharmacist’s intervention on humanistic, clinical and economic outcomes in patients with CVD [94].
A clinical pharmacist prepared for smoking cessation counseling can play a key job in giving such mediations, including the evaluation of pharmacotherapy interactions with tobacco smoke [103]. Prescription smoking cessation medications include bupropion and varenicline [104]. A recent Canadian survey shows that pharmacist-led intervention resulted in more than 70% of patients using nicotine replacement therapy for smoking cessation [105] Figure 3.
Obesity Management
In each nation on the earth, the rate of obesity is rising constantly with coronary artery disease, hypertension, type 2 diabetes mellitus, respiratory disorders and dyslipidemia [106]. The WHO assessed that in 2016 more than 1.9 billion grown-ups were overweight (almost 40% of the population) and more than 650 million (13% of the population) were people with heftiness [107]. Globally, the yearly cost of corpulence related diseases has come to $2 trillion as per an ongoing report by McKinsey Global Institute [108]. Corpulence expands cardiovascular risk through risk factors, for example, expanded fasting plasma triglycerides, high LDL cholesterol, low HDL cholesterol, raised blood glucose and insulin levels and hypertension [109,110]. Likewise, obesity causes cerebral vasculopathy, gallbladder lithiasis, arthropathy, ovarian polycystic, sleep apnea syndrome, and a few neoplasms [111].
Successful obesity treatment plans incorporate diet, exercise, behavior modification (with or without drug treatment), and/or surgical intervention [112]. Prior to recommending any treatment, the clinician must evaluate the patient for the presence of secondary causes of obesity, such as thyroid dysfunction [113,114]. If secondary causes are suspected, then a more complete diagnostic workup and appropriate therapy is important. The clinician should then evaluate the patient for the presence and severity of other obesityrelated diseases, evaluating appropriate lab tests as indicated. Based on the outcome of this medical evaluation, the patient should be counseled on the risks and benefits of available treatment options (along with obesity‐related comorbidities, including T2D prevention, and improvements in dyslipidemia, hyperglycemia, osteoarthritis, stress incontinence, GERD, hypertension, and PCOS [115,116]. If obesity is present without other comorbid conditions, then the goal would be absolute weight loss. In the presence of comorbid conditions, relatively small reductions in total body weight can have significant effects on comorbidity [117] Figure 4.
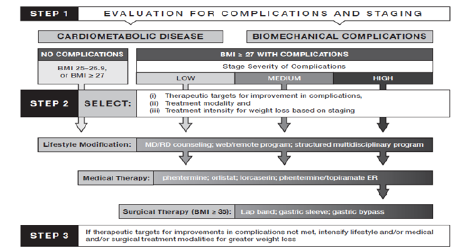
Figure 4:2013 AACE Obesity Treatment Algorithm [118].
Pharmacists, regularly viewed as one of the most dependable and open healthcare professionals, are in a perfect world arranged to give counseling to weight and way of life management. All around prepared pharmacists to perform fundamental physical evaluations, for example, weight, abdomen circumference, blood glucose monitoring, and pharmacotherapy counseling, while extra training could be effectively acquired for administrations that would incorporate dietary counseling, direction on physical activity, and behavioral counseling [108], [119,120]. As pharmacists currently do not have a well-identified role in obesity management, but study results display that pharmacist intervention was beneficial [121].
According to Canadian Pharmacists Journal, 2016 pharmacist prescribing resulted in >3-fold more patients achieving target LDL-c levels [[122]]. Pharmacists who identify and treat patients with dyslipidemia, including those with inadequately controlled LDL cholesterol levels, are better than physicians at getting patients to goal [123]. Studies have demonstrated that pharmacistled interventions, including lipid clinics, can help patients achieve these more aggressive goals [124,125].
Asthma & COPD management
Asthma and COPD are common chronic conditions that comprise nearly 80% of direct health care costs associated with respiratory diseases in the EU [126]. In the UK alone, 5.4 million patients are currently receiving treatment for asthma; of these, 1.1 million are children. Over three million people die of COPD worldwide each year, an estimated 6% of all deaths worldwide [127]. It is the second most common reason for emergency hospital admission. According to WHO, COPD has become the fourth leading cause of mortality in the US. It is estimated to become the fifth leading cause of disease burden in 2020 [128]. In 2015 alone, the death toll due to asthma was 383,000 globally [129]. One in five individuals with a diagnosis of COPD, asthma, or both asthma and COPD in primary care settings have asthma-COPD overlap [130]. In COPD, the outpatient therapeutic and management goals are to reduce symptoms and risks from exacerbations, and to maintain drug therapy. In contrast with asthma, COPD is a disease caused by chronic and often daily exposure to noxious particles or gases. The small airways in COPD are gradually destroyed leading to chronic bronchitis and emphysema [131].
Ideal pharmacological treatment including fast treatment of exacerbations, can improve symptoms, diminish exacerbation recurrence, and improve practice resilience, while poor medication adherence and imperfect inhaler technique contrarily sway outcomes [132]. Adherence to breathed in medication is poor and shows extraordinary inconstancy, going from as low as 20% to over 60% [133]. To improve adherence, the therapeutic choices ought to be talked about with the patient and should contemplate their lifestyle factors, demographic attributes (age, co-morbidities, physical confinements, mental and cognitive status), and pharmacological factors (polypharmacy regimens) to pick the best inhaler device for that patient [134]. Pharmacist-led comprehensive therapeutic interchange program of COPD inhalers may provide 30% pharmacy cost savings, improved medication adherence, knowledge of disease, decrease the number of prescriptions for exacerbations for these patients. and reduces 30-day readmission rate [135-138]. A pharmacist-driven spirometry service was associated with quality testing results, identified respiratory disease abnormalities, and helped modifications of pulmonary drug regimens based on evidence-based guidelines [137].
Despite advances in inhaler device technology, estimates of those making inhaler errors range up to 90% of patients irrespective of the device type used. Poor inhaler technique accounted for over €750 million in direct and indirect costs in 2015 in the UK, Spain and Sweden [39]. By providing pharmaceutical care to patients with asthma, the pharmacist can help them to achieve treatment goals, e.g. improvement of disease control and reduction of asthma symptoms, exacerbations and medication-related side effects [140]. Step up therapy contained expanding or beginning corticosteroid/ long-acting beta agonist mix inhaler; corticosteroid inhaler; shortacting muscarinic antagonist inhaler; oral corticosteroid; oral montelukast; or long-acting muscarinic antagonist inhaler. Step down of therapy included diminishing or halting corticosteroid/ long-acting beta agonist mix inhaler; corticosteroid inhaler; or long-acting muscarinic antagonist inhaler. The pharmacist directed exercises, for example, giving asthma activity plans, instructing patients, prescribing to step up/down therapy, auditing inhaler technique and making other significant proposals, for example, gadget changes (e.g., dry-powder to metered-dose inhaler) [141]. Polypharmacy is oppressive and related with patients hospitalized with intense intensifications. It is conceivable that rehashed pharmacist intervention to guarantee ideal pharmacotherapy and limit adverse effects, with an immediate connect to a consultant respiratory physician, and the patient’s GP, may prompt improved results [142]. The interventions identified focused on key areas of asthma and COPD management and support including assessment of current symptoms; assessment and rectification of inhaler technique; identification of medication-related problems; medication adherence; provision of written and oral education materials; smoking cessation [143] Figure 5.
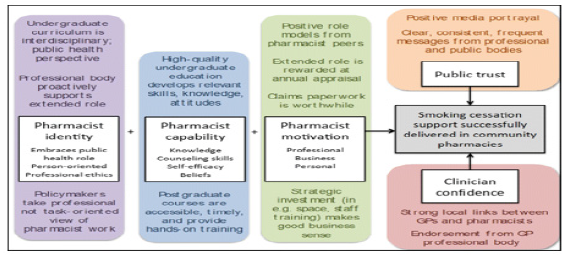
Figure 5:Unifying models showing key influences on successful delivery of smoking cessation support by pharmacists [144].
Osteoporosis
Around the world, it is evaluated that 1 of every 3 women over the age of 50 will encounter osteoporotic fractures, just as 1 out of 5 men [145]. The predominance of osteoporosis is anticipated to ascend in the US from around 10 million individuals to in excess of 14 million individuals by 2020 [146]. In 2015, direct medical costs totaled $637.5 million for lethal fall injuries and $31.3 billion for nonfatal fall injuries. During that year, hospitalizations cost a normal of $30,550 per fall affirmation, totaling $17.8 billion. By 2025, the expense of fractures in the US is relied upon to surpass $25 billion every year to treat in excess of 3,000,000 anticipated fractures [147]. Like other chronic diseases, osteoporosis has struggled with prescription non-adherence, bringing about an expanded danger of fractures and all-cause mortality. The gaps in osteoporosis management are all well-documented: (a) most patients at high chance for break are not recognized for treatment, and (b) adherence to osteoporosis pharmacotherapy is imperfect [148]. About half osteoporosis patients are non-disciple to medications. Besides, around 50-70% of the patients stop their osteoporosis medications inside the main year of commencement, which results in expanded horribleness and mortality [149]. In October 2010, the US FDA issued a safety communication regarding the risks of atypical fractures of the femur, with bisphosphonates drugs, the safety communication appeared to have influenced osteoporosis utilization in Medicaid recipients [150] Figure 6.
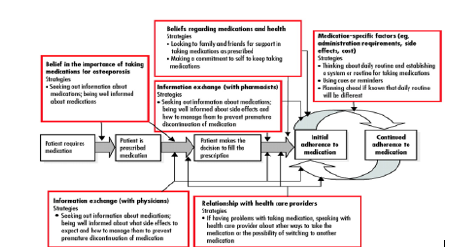
Figure 6: Mapping the factors influencing adherence and adherence strategies onto the medication-taking process in patients with osteoporosis [151].
High patient cost and safety concerns are barriers for nearly 60% patients [152]. Improved osteoporosis medication adherence can reduce osteoporosis-related health care costs by preventing fractures. Persistent pharmacotherapy for osteoporosis is necessary to prevent osteoporotic fractures and to reduce osteoporosis related health care costs [153]. Treatment strategies of osteoporosis include non-pharmacological treatment diet rich of calcium and vitamin D, healthy lifestyle, proper exercise plan, and pharmacological therapy [154]. BMD monitoring after initiating anti-osteoporosis therapy in the routine clinical practice setting [155]. Hypercalciuria, malabsorption of calcium, hyperparathyroidism, vitamin D deficiency, hyperthyroidism, Cushing’s disease, and hypocalciuric hypercalcemia attributed to secondary causes to more than 30% women. Disorders of calcium metabolism and hyperparathyroidism contributed to nearly 80% of the secondary causes [156]. Hormone replacement therapy (HRT) is not first-line therapy position for osteoporosis but is best for prevention of osteoporosis [157]. However, different types of estrogen or progestogen, as well as different formulations, doses, timing of initiation, durations of therapy, and patient characteristics, may play different roles in the effects of HRT [158]. Pharmacistphysician collaboration is associated with higher treatment rates of osteoporosis [159]. Physicians and pharmacist should invest time to educate patients about the potential side effects and box warnings of estrogen use. Routine women wellness exams should also be focused on the development of any malignancies or adverse effects of hormone replacement therapy given a positive history. The pharmacist can play an important role at multiple levels: supporting patients in treatment, by providing information on the disease, its treatment, proper use of medication, adherence and persistence, as well as raising awareness for the prevention of osteoporosis and identifying patients at risk [160]. The counseling should include educating and assessing the patient for proper use of estrogen medication therapies as they may be prescribed in many various preparations of oral, transdermal, vaginal insert, and topic vaginal creams for positive patient compliance and adherence to therapy [147].
Inflammatory Bowel Disease (IBD)
Inflammatory bowel disease (IBD) is a group of inflammatory conditions of the colon and small intestine. The two most common diseases are ulcerative colitis and Crohn’s disease (CD). Crohn’s disease can cause inflammation in any part of the digestive tract. Ulcerative colitis (UC) is an idiopathic inflammatory condition of the colon which results in diffuse friability and superficial erosions on the colonic wall associated with bleeding [161]. Although these diseases have undetermined etiology, research advances have outlined some of the pathways by which they occur: a) genetic predisposition associated with the environment induces a disruption of the intestinal microbial flora, b) the epithelial cells and the immune system of the intestine itself determine the risk of developing the disease [162]. Treatment of both, IBD and IBD associated pain is challenging. The mainstay of IBD treatment includes systemic immunosuppressive medications, such as corticosteroids, anti-tumor TNF antibodies or immunomodulators. Furthermore, the management of an acute flare differs from the strategies for maintenance of remission [163]. A total of about 66,000 US residents with a new IBD diagnosis each year, since 2015 [164]. Direct costs (including consultations, drugs, hospitalization and surgery) of UC amount to $3.4-$8.6 billion in the US and €5.4- €12.6 billion in EU [165]. The prevalent populations of patients with CD or UC in the UC in 2016 are expected to incur lifetime total costs of $498 billion and $377 billion, respectively [166]. IBD is a relapsing-remitting condition that causes inflammation and ulceration in the bowels, affecting approximately 500,000 people in the UK [167] Figure 7.
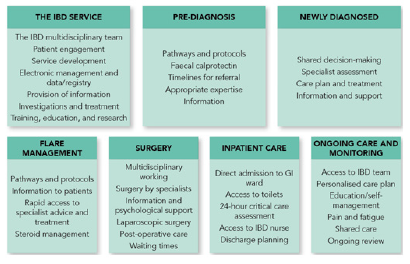
Figure 7:The seven sections of the 2019 IBD Standards [167].
The increasing incidence of IBD in developing countries parallels the westernization of diet, which includes higher calorie intake, especially from sugar, refined carbohydrates, animal proteins and ultra-processed foods and a lesser intake of fiber and fruits [168,169]. Incidence rate of IBD is stabilizing in some developed countries; however, the incidence rate is increasing in developing countries such as Asia and Eastern Europe [170]. Anxiety and depression are the most common psychological disorders in patients with IBD [171]. IBD is associated with significantly increased MI compared with non-IBD patients [172]. Patients with IBD are also at risk for asthma or COPD and bronchiectasis [173,174]. Sacroiliitis, an inflammatory arthropathy associated with ankylosing spondylitis, is found in patients with IBD but may go undiagnosed [175]. IBD patients showed increased risk for lymphoma and biliary cancer [176]. The general objectives of treatment are to instigate and maintain remission, limit intricacies and sickness manifestations, and improve overall QoL. Customized IBD pharmacist adherence counseling, considering the Health Beliefs Model of prescription recognition, may expand drug adherence. Instruction utilizing pamphlets and ad hoc physician training improved information yet not adherence [177]. IBD patients, fundamentally those having UC, need medications for a mind-blowing duration with periodic dosing and occasionally, enemas and infusions may likewise be required. Treatment without adherence is exceptionally viewed as the noteworthy factor for relapse occurrence [[178]].
Prescription nonadherence in IBD can be improved through a solitary customized counseling session by IBD pharmacist adherence counseling (IPAC) intervention, and the advantage was sturdy for a long time [179]. In addition to the ailment, these patients are likewise dealt with powerful medications like steroids and biological agents, which have a large group of adverse effects. Along these lines, the significance of the pharmacist who ought to be alert for any adverse reaction [180]. Pharmacist-led drug monitoring clinics measure thioguanine nucleotides and thiopurine methyltransferase levels four weeks after treatment with thiopurines is started to optimize outcomes [181]. If insurance coverage can’t be acquired for the chose biologic response modifiers, the pharmacist recognizes and talks about elective alternatives with the GI team; a portion of these choices may incorporate changing to another model operator or selecting patients in medicine assistance programs. When insurance coverage of the medicine is verified, the pharmacist teaches the patient on self-administration, stability and storage prerequisites, and potential adverse effects. Additionally, the pharmacist features the noteworthiness of consistence with laboratory monitoring and reviews the significance of speaking with the GI team in the event of potential infection, exacerbating sickness control, or issues getting or utilizing the medicine
The IBD pharmacist has a key job in the administration of IBD patients contributing not exclusively to drug monitoring, recommending, and wellbeing yet in addition allowing more prominent limit in the physician’s, frequently profoundly stretched IBD clinics [182]. Past drug therapy coordination from start to finish, the pharmacist assumes a functioning job in helping with medicine reconciliation and guaranteeing patients are present on essential immunizations [183]. 40% of patients with CD do not respond to treatment with biologics, 30%-50% achieve complete remission after six months and 30% of patients maintain the response for 12months with continual treatment. Current strategies to overcome loss of response involve increasing the dose, decreasing the interval between administrations or switching to an alternative agent [181].
Conclusion
The pharmacist’s fundamental obligation is to augment positive results of drug therapy and limit drug misadventures. Patient therapy should bring about the achievement of definite results that improve the patient’s QoL. Until now, various examinations have discovered an expanded pace of clinic admission rates optional to medicine rebelliousness as well as adverse drug reactions. The genuine number of DRPs requiring clinic admission might be higher than revealed because of absence of documentation, further underestimating the issue. Initially, gathering and deciphering pertinent patient information, identifying patient social insurance needs, and planning a DRP rundown might challenge for the pharmacist. Preventive or chronic consideration is a challenge that ought to be embraced by social insurance suppliers in all training settings. Pharmacists should “seize the moment” to teach and insight patients with respect to these different points when the open doors emerge. Clinical pharmacists use populace wellbeing techniques to create chronic infection the management referrals for patients with uncontrolled chronic conditions. Open doors for pharmacists to help realize consciousness of recommendations and hazard factors for the development of disease and instruct patients with regards to the advantages of prevention, happen every day. It is significant for the pharmacists on the “bleeding edge” to have a general comprehension of ebb and flow recommendations for screening and sickness prevention with the goal that they can give proper counseling and care to their patients. Also, pediatric clinical pharmacists have evolved over the last 2 decades and have proven to be a key player in the multidisciplinary team. Although, there are ample of evidences of positive impact on clinical, humanistic and economic outcomes and the benefits of clinical pharmacists managing chronic conditions have been extensively published, their involvement in the multidisciplinary team providing care to patients with chronic cases, more high-quality research is warranted.
Acknowledgement
I’m thankful to Dr. Christel G. Svingen, Deputy Director of Pharmacy Red Lake Indian Health Service Hospital, Minnesota for his valuable time to audit my paper and for his thoughtful suggestions. I’m also grateful to seminar library of Faculty of Pharmacy, University of Dhaka and BANSDOC Library, Bangladesh for providing me books, journal and newsletters.
Conflict-of-Interest
The author declares that he has no competing interests.
References
- Miller RR (1981) History of clinical pharmacy and clinical pharmacology. J Clin Pharmacol 21(4): 195-197.
- Somogyi A, Loke YK, Ferro A, Lewis LD, Cohen AF, et al. (2010) Clinical pharmacology: a declaration of intent. Br J Clin Pharmacol 70(1): 1-2.
- Calvert RT (1999) Clinical pharmacy-a hospital perspective. Br J Clin Pharmacol 47(3): 231-238.
- Carter BL (2016) Evolution of Clinical Pharmacy in the USA and Future Directions for Patient Care Drugs Aging 33(3): 169-177.
- Dhingra S, Kumria R (2014) A case report on the significance of clinical pharmacy services in India. Clin Case Rep 2(3): 86-87.
- Lebovitz L, Eddington ND (2019) Trends in the Pharmacist Workforce and Pharmacy Education. Am J Pharm Educ 83(1): 7051.
- Veggeland T, Dyb S (2008) The contribution of a clinical pharmacist to the improvement of medication at a geriatric hospital unit in Norway. Pharm Pract (Granada) 6(1): 20-24.
- Horn E, Jacobi J (2006) The critical care clinical pharmacist: evolution of an essential team member. Crit Care Med 34(3): 46-51.
- Hazen ACM, de Bont AA, Leendertse AJ, Zwart DLM, de Wit NJ, et al. (2019) How Clinical Integration of Pharmacists in General Practice has Impact on Medication Therapy Management: A Theory-oriented Evaluation. Int J Integr Care 19(1): 1.
- Islam MA, Talukder RM, Taheri R, Blanchard N (2016) Integration of Basic and Clinical Science Courses in US PharmD Programs. Am J Pharm Educ 80(10): 166.
- (2008) American College of Clinical Pharmacy. The definition of clinical pharmacy. Pharmacotherapy 28(6): 816-817.
- McCarthy MW (2009) Chapter 4. Clinical Pharmacy Skills. In; Michelle McCarthy and Denise Kockler. Oxford American Handbook of Clinical Pharmacy, published by Oxford University Press 1 edition
- (2009) Institute of Medicine (US) Roundtable on Evidence-Based Medicine. Leadership Commitments to Improve Value in Healthcare: Finding Common Ground: Workshop Summary.
- Knoer SJ, Eck AR, Lucas AJ (2016) A review of American pharmacy: education, training, technology, and practice. J Pharm Health Care Sci 9(2): 32.
- Ma CS, Holuby RS, Bucci LL (2010) Physician and pharmacist collaboration: The University of Hawaii at Hilo College of Pharmacy--JABSOM experience. Hawaii Med J 69(63): 42-44.
- Svingen CG (2019) Clinical Pharmacist Credentialing and Privileging: A Process for Ensuring High-Quality Patient Care. Fed Pract 36(4): 155-157.
- Ismail S, Osman M, Abulezz R, Alhamdan H, Quadri KHM (2018) Pharmacists as Interprofessional Collaborators and Leaders through Clinical Pathways. Pharmacy (Basel) 6(1): 24.
- Ascione FJ (2019) Preparing Pharmacists for Collaborative/Integrated Health Settings. Pharmacy (Basel) 7(2): 47.
- Moreno G, Lonowski S, Fu J, Chon JS, Whitmire N, et al. (2017) Physician experiences with clinical pharmacists in primary care teams. J Am Pharm Assoc (2003) 57(6): 686-691.
- Al-Taani GM, Al-Azzam SI, Alzoubi KH, Aldeyab MA (2018) Which drugs cause treatment-related problems? Analysis of 10, 672 problems within the outpatient setting. Ther Clin Risk Manag 14: 2273-2281.
- Mohiuddin AK. (2019) “Pharmacists in Public Health: Scope in Home and Abroad.” SOJ Pharmacy & Pharmaceutical Sciences 6(1): 1-23.
- Toklu HZ, Hussain A (2013) The changing face of pharmacy practice and the need for a new model of pharmacy education. J Young Pharm 5(2): 38-40.
- Sakeena MHF, Bennett AA, McLachlan AJ (2019) The Need to Strengthen the Role of the Pharmacist in Sri Lanka: Perspectives. Pharmacy (Basel) 7(2): 54.
- Hammad EA, Qudah RA, Akour AA (2017) The impact of clinical pharmacists in improving Jordanian patients' health outcomes. Saudi Med J 38(11): 1077-1089.
- Dalton K, Byrne S (2017) Role of the pharmacist in reducing healthcare costs: current insights. Integr Pharm Res Pract 6: 37-46.
- Li J, Li Z (2018) Differences and similarities in clinical pharmacy practice in China and the United States: a narrative review. Eur J Hosp Pharm 25(1): 2-5.
- Tripathi S, Crabtree HM, Fryer KR, Graner KK, Arteaga GM (2015) Impact of Clinical Pharmacist on the Pediatric Intensive Care Practice: An 11-Year Tertiary Center Experience. J Pediatr Pharmacol Ther 20(4): 290-298.
- Mekonnen AB, Yesuf EA, Odegard PS, Wega SS (2013) Implementing ward based clinical pharmacy services in an Ethiopian University Hospital. Pharm Pract (Granada) 11(1): 51-7.
- Francis J, Abraham S (2014) Clinical pharmacists: Bridging the gap between patients and physicians. Saudi Pharm J 22(6): 600-602.
- Chalasani SH, Ramesh M, Gurumurthy P (2018) Pharmacist-Initiated Medication Error-Reporting and Monitoring Programme in a Developing Country Scenario Pharmacy (Basel) 6(4): 133.
- Ernawati DK, Lee YP, Hughes JD (2014) Nature and frequency of medication errors in a geriatric ward: an Indonesian experience. Ther Clin Risk Manag 10: 413-421.
- Chamoun NR, Zeenny R, Mansour H (2016) Impact of clinical pharmacy interventions on medication error nodes. Int J Clin Pharm 38(6): 1436-1444.
- Gonzalez D, Rao GG, Bailey SC, Brouwer KLR, Cao Y, et al. (2017). Precision Dosing: Public Health Need, Proposed Framework, and Anticipated Impact. Clin Transl Sci 10(6): 443-454.
- Sanii Y, Torkamandi H, Gholami K, Hadavand N, Javadi M (2016) Role of pharmacist counseling in pharmacotherapy quality improvement. J Res Pharm Pract 5(2): 132-137.
- Ip RNS, Tenney JW, Chu ACK, Chu PLM, Young GWM (2018) Pharmacist Clinical Interventions and Discharge Counseling in Medical Rehabilitation Wards in a Local Hospital: A Prospective Trial Geriatrics (Basel) 3(3): 53.
- Seidling HM, Lampert A, Lohmann K, Schiele JT, Send AJ, et al. (2013) Safeguarding the process of drug administration with an emphasis on electronic support tools. Br J Clin Pharmacol 76(1): 25-36.
- Bauer SR, Kane-Gill SL (2016) Outcome Assessment of Critical Care Pharmacist Services. Hosp Pharm; 51(7): 507-513.
- Viana SSC, Arantes T, Ribeiro SCDC (2017) Interventions of the clinical pharmacist in an Intermediate Care Unit for elderly patients. Einstein Sao Paulo 15(3): 283-288.
- Sjölander M, Gustafsson M, Gallego G (2017) Doctors' and nurses' perceptions of a ward-based pharmacist in rural northern Sweden. Int J Clin Pharm 39(4): 953-959.
- Van Oostrom SH, Picavet HS, de Bruin SR, Stirbu I, Korevaar JC, et al. (2014) Multimorbidity of chronic diseases and health care utilization in general practice BMC Fam Pract 15: 61.
- Yi JY, Kim Y, Cho YM, Kim H (2018) Self-management of Chronic Conditions Using mHealth Interventions in Korea: A Systematic Review. Healthc Inform Res 24(3): 187-197.
- Kent K, Johnson JD, Simeon K, Frates EP (2016) Case Series in Lifestyle Medicine: A Team Approach to Behavior Changes. Am J Lifestyle Med 10(6): 388-397.
- Middleton KR, Anton SD, Perri MG (2013) Long-Term Adherence to Health Behavior Change. Am J Lifestyle Med 7(6): 395-404.
- Young S (2014) Healthy behavior change in practical settings. Perm J Fall 18(4): 89-92.
- Newsom JT, Huguet N, McCarthy MJ, Ramage-Morin P, Kaplan MS, et al. (2012) Health behavior change following chronic illness in middle and later life. J Gerontol B Psychol Sci Soc Sci 67(3): 279-288.
- Zhang C, Zhang L, Huang L, Luo R, Wen J (2012) Clinical pharmacists on medical care of pediatric inpatients: a single center randomized controlled trial. PLoS One 7(1): 30856.
- Han N, Han SH, Chu H, Kim J, Rhew KY, et al. (2018) Drug TEAM Study group. Service design oriented multidisciplinary collaborative team care service model development for resolving drug related problems. PLoS One 13(9): 0201705.
- Tan EC, Stewart K, Elliott RA, George J (2014) Pharmacist services provided in general practice clinics: a systematic review and meta-analysis. Res Social Adm Pharm 10(4): 608-622.
- Fletcher J, Hogg W, Farrell B, Woodend K, Dahrouge S, et al. (2012) Effect of nurse practitioner and pharmacist counseling on inappropriate medication use in family practice. Can Fam Physician 58(8): 862-868.
- Greer N, Bolduc J, Geurkink E, Rector T, Olson K, et al. (2016) Pharmacist-led Chronic Disease Management: A Systematic Review of Effectiveness and Harms Compared with Usual Care. Ann Intern Med.
- Litke J, Spoutz L, Ahlstrom D, Perdew C, Llamas W, et al. (2018) Impact of the clinical pharmacy specialist in telehealth primary care. Am J Health Syst Pharm 75(13): 982-986.
- Meo SA, Sheikh SA, Sattar K, Akram A, Hassan A, et al. (2019) Prevalence of Type 2 Diabetes Mellitus Among Men in the Middle East: A Retrospective Study. Am J Mens Health 13(3): 1557988319848577.
- Hughes JD, Wibowo Y, Sunderland B, Hoti K (2017) The role of the pharmacist in the management of type 2 diabetes: current insights and future directions. Integr Pharm Res Pract 6: 15-27.
- Muc R, Saracen A, Grabska-Liberek I (2018) Associations of Diabetic Retinopathy with Retinal Neurodegeneration on the Background of Diabetes Mellitus. Overview of Recent Medical Studies with an Assessment of the Impact on Healthcare systems. Open Med Wars 13: 130-136.
- Yang Jae Jeong, Yu D, Wen W, Saito E, Rahman S et al. (2019) “Association of Diabetes with All-Cause and Cause-Specific Mortality in Asia: A Pooled Analysis of More Than 1 Million Participants.” JAMA netw open (4):
- Raghavan S, Vassy JL, Ho YL, Song RJ, Gagnon DR, et al. (2019) Diabetes Mellitus-Related All-Cause and Cardiovascular Mortality in a National Cohort of Adults. J Am Heart Assoc 8(4): 011295.
- Einarson TR, Acs A, Ludwig C, Panton UH (2018) Prevalence of cardiovascular disease in type 2 diabetes: a systematic literature review of scientific evidence from across the world in 2007-2017. Cardiovasc Diabetol 17(1): 83.
- Longo M, Bellastella G, Maiorino MI, Meier JJ, Esposito K, et al (2019) Diabetes and Aging: From Treatment Goals to Pharmacologic Therapy. Front Endocrinol (Lausanne) 10: 45.
- Ares J, Valdés S, Botas P, Sánchez-Ragnarsson C, Rodríguez-Rodero S et al. (2019) Mortality risk in adults according to categories of impaired glucose metabolism after 18 years of follow-up in the North of Spain: The Asturias Study. PLoS One 14(1): 0211070.
- Mohiuddin AK (2019) Patient Compliance: Fact or Fiction? INNOVATIONS in pharmacy 10(1):1-13.
- Al-Omar LT, Anderson SL, Cizmic AD, Vlasimsky TB (2019) Implementation of a Pharmacist-Led Diabetes Management Protocol. Am Health Drug Benefits 12(1): 14-20.
- Gardea J, Papadatos J, Cadle R (2018) Evaluating glycemic control for patient-aligned care team clinical pharmacy specialists at a large Veterans Affairs medical center. Pharm Pract (Granada) 16(2): 1164.
- Shane-McWhorter L, McAdam-Marx C, Lenert L, Petersen M, Woolsey S, et al. (2015) Pharmacist-provided diabetes management and education via a telemonitoring program. J Am Pharm Assoc (2003) 55(5): 516-526.
- Davis CS, Ross LAR, Bloodworth LS (2017) The Impact of Clinical Pharmacist Integration on a Collaborative Interdisciplinary Diabetes Management Team. J Pharm Pract 30(3): 286-290.
- Wallgren S, Berry-Cabán CS, Bowers L (2012) Impact of clinical pharmacist intervention on diabetes-related outcomes in a military treatment facility. Ann Pharmacother 46(3): 353-357.
- Ray S, Lokken J, Whyte C, Baumann A, Oldani M (2019) The impact of a pharmacist-driven, collaborative practice on diabetes management in an Urban underserved population: a mixed method assessment. J Interprof Care 5: 1-9.
- Schmidt K, Caudill JA, Hamilton T (2019) Impact of clinical pharmacy specialists on glycemic control in veterans with type 2 diabetes. Am J Health Syst Pharm 76(1): 9-14.
- Sharp LK, Tilton JJ, Touchette DR, Xia Y, Mihailescu D, et al. (2018) Community Health Workers Supporting Clinical Pharmacists in Diabetes Management: A Randomized Controlled Trial. Pharmacotherapy 38(1): 58-68.
- Neves CM, Nascimento MMGD, Silva DÁM, Ramalho-de-Oliveira D (2019) Clinical Results of Comprehensive Medication Management Services in Primary Care in Belo Horizonte. Pharmacy (Basel) 7(2): 58.
- Jeong S, Lee M, Ji E (2018) Effect of pharmaceutical care interventions on glycemic control in patients with diabetes: a systematic review and meta-analysis. Ther Clin Risk Manag 14: 1813-1829.
- Wassell K, Sullivan J, Jett BP, Zuber J. Comparison of clinical pharmacy specialists and primary care physicians in treatment of type 2 diabetes mellitus in rural Veterans Affairs facilities. Am J Health Syst Pharm 75(51): 6-12.
- Kharjul M, Braund R, Green J (2018) The influence of pharmacist-led adherence support on glycaemic control in people with type 2 diabetes. Int J Clin Pharm 40(2): 354-359.
- Alqudah S, Jarab AS, Alefishat EA, Mayyas F, Khdour M, et al. (2019) Factors Associated with Poor Hemoglobin A1c Control in Patients with Type 2 Diabetes. Curr Diabetes Rev 15(2): 164-170.
- Peasah SK, Granitz K, Vu M, Jacob B (2019) Effectiveness of a Student Pharmacist-Led Telephone Follow-Up Intervention to Improve Hemoglobin A(1C) in Diabetic Patients. J Pharm Pract: 897190019857409.
- Goruntla N, Mallela V, Nayakanti D (2019) Impact of Pharmacist-directed Counseling and Message Reminder Services on Medication Adherence and Clinical Outcomes in Type 2 Diabetes Mellitus. J Pharm Bioallied Sci 11(1): 69-76.
- Al Haqan AA, Al-Taweel DM, Awad A, Wake DJ (2017) Pharmacists' Attitudes and Role in Diabetes Management in Kuwait. Med Princ Pract 26(3): 273-279.
- Bukhsh A, Khan TM, Lee SWH, Lee LH, Chan KG, et al. (2018) Efficacy of Pharmacist Based Diabetes Educational Interventions on Clinical Outcomes of Adults with Type 2 Diabetes Mellitus: A Network Meta-Analysis. Front Pharmacol 9: 339.
- Okubadejo NU, Ozoh OB, Ojo OO, Akinkugbe AO, Odeniyi IA, et al. (2019) Prevalence of hypertension and blood pressure profile amongst urban-dwelling adults in Nigeria: a comparative analysis based on recent guideline recommendations. Clin Hypertens 25: 7.
- Web WHO. Cardiovascular disease. World Heart Day. Scale up prevention of heart attack and stroke.
- Web WHO. News/ Fact sheets/Detail/Cardiovascular diseases (CVDs).
- Ofori SN, Obosi J (2019) Prevalence of hypertension among office workers in a multi-national company in the Niger-Delta with the 2017 American College of Cardiology/American Heart Association Blood Pressure Guidelines. Prev Med Rep 15:100899.
- Lanza GA (2019) Diagnostic Approach to Patients with Stable Angina and No Obstructive Coronary Arteries. Eur Cardiol 14(2): 97-102.
- Yasue H, Mizuno Y, Harada E (2019) Coronary artery spasm - Clinical features, pathogenesis and treatment. Proc Jpn Acad Ser B Phys Biol Sci 95(2): 53-66.
- Ferdinand KC, Senatore FF, Clayton-Jeter H, Cryer DR, Lewin JC, et al. (2017) Improving Medication Adherence in Cardiometabolic Disease: Practical and Regulatory Implications. J Am Coll Cardiol 69(4): 437-451.
- Hinton W, McGovern A, Coyle R, Han TS, Sharma P, et al. (2018) Incidence and prevalence of cardiovascular disease in English primary care: a cross-sectional and follow-up study of the Royal College of General Practitioners (RCGP) Research and Surveillance Centre (RSC). BMJ Open 8(8): 020282.
- Mohiuddin Ak (2019) “Natural Foods and Indian Herbs of Cardiovascular Interest.” Pharmacy & Pharmacology International Journal 7(2).
- Gums TH, Uribe L, Vander Weg MW, James P, Coffey C, et al. (2015) Pharmacist intervention for blood pressure control: medication intensification and adherence. J Am Soc Hypertens; 9(7): 569-578.
- Mohiuddin AK (2019) “Risks and Reasons Associated with Medication Non-Adherence.” Journal of Clinical Pharmacy 1(1): 50-53.
- Williams B, Mancia G, Spiering W, Agabiti Rosei E, Azizi M, et al. (2018) 2018 ESC/ESH Guidelines for the management of arterial hypertension. Eur Heart J 39(33): 3021-3104.
- Niriayo YL, Ibrahim S, Kassa TD, Asgedom SW, Atey TM, et al. (2019) Practice and predictors of self-care behaviors among ambulatory patients with hypertension in Ethiopia. PLoS One 14(6): 0218947.
- (2004) National High Blood Pressure Education Program. The Seventh Report of the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure. Bethesda (MD): National Heart, Lung, and Blood Institute (US).
- Mohiuddin AK (2019) A Brief Review of Traditional Plants as Sources of Pharmacological Interests. Open Journal of Plant Science pp. 1-8.
- Mohiuddin AK (2019) Traditional System of Medicine and Nutritional Supplementation: Use Vs Regulation. Journal of Clinical Trials, Pathology and Case Studies 4(1): 5-30.
- Mohiuddin AK (2019) Patient History and Medical Record: Proper Solution from Accurate Problem Identification. Medicine and Medical Sciences 7(7): 82-86.
- Omboni S, Caserini M (2018) Effectiveness of pharmacist's intervention in the management of cardiovascular diseases. Open Heart 5(1): 687.
- Morgado M, Rolo S, Castelo-Branco M (2011) Pharmacist intervention program to enhance hypertension control: a randomised controlled trial. Int J Clin Pharm 33(1): 132-140.
- Bex SD, Boldt AS, Needham SB, Bolf SM, Walston CM, et al. (2011) Effectiveness of a hypertension care management program provided by clinical pharmacists for veterans. Pharmacotherapy 31(1): 31-38.
- Von Muenster SJ, Carter BL, Weber CA, Ernst ME, Milchak JL, et al. (2008) Description of pharmacist interventions during physician-pharmacist co-management of hypertension. Pharm World Sci 30(1): 128-135.
- Ramanath K, Balaji D, Nagakishore Ch, Kumar SM, Bhanuprakash M (2012) A study on impact of clinical pharmacist interventions on medication adherence and quality of life in rural hypertensive patients. J Young Pharm 4(2): 95-100.
- Bhat S, Kroehl M, Yi WM, Jaeger J, Thompson AM, et al. (2003) Factors influencing the acceptance of referrals for clinical pharmacist managed disease states in primary care. J Am Pharm Assoc 59(3): 336-342.
- Kane JA, Mehmood T, Munir I, Kamran H, Kariyanna PT, et al. (2019) Cardiovascular Risk Reduction Associated with Pharmacological Weight Loss: A Meta-Analysis. Int J Clin Res Trials 4(1): 131.
- Hasegawa K, Komiyama M, Takahashi Y (2019) Obesity and Cardiovascular Risk After Quitting Smoking: The Latest Evidence. Eur Cardiol 14(1): 60-61.
- El Hajj MS, Kheir N, Al Mulla AM, Shami R, Fanous N, et al. (2017) Effectiveness of a pharmacist-delivered smoking cessation program in the State of Qatar: a randomized controlled trial. BMC Public Health 17(1): 215.
- Dobrinas M, Blanc AL, Rouiller F, Christen G, Coronado M, et al. (2014) Clinical pharmacist's role in implementing a smoking cessation intervention in a Swiss regional hospital: an exploratory study. Int J Clin Pharm 36(3): 526-534.
- El Hajj MS, Awaisu A, Kheir N, Mohamed MHN, Haddad RS, et al. (2019) Evaluation of an intensive education program on the treatment of tobacco-use disorder for pharmacists: a study protocol for a randomized controlled trial. Trials 20(1): 25.
- Li VW, Lam J, Heise P, Reid RD, Mullen KA (2018) Implementation of a Pharmacist-Led Inpatient Tobacco Cessation Intervention in a Rehabilitation Hospital: A Before-and-After Pilot Study. Can J Hosp Pharm 71(3): 180-186.
- Klop B, Elte JW, Cabezas MC (2013) Dyslipidemia in obesity: mechanisms and potential targets. Nutrients 5(4): 1218-1240.
- Cercato C, Fonseca FA (2019) Cardiovascular risk and obesity. Diabetol Metab Syndr 11:74.
- Jordan MA, Harmon J (2015) Pharmacist interventions for obesity: improving treatment adherence and patient outcomes. Integr Pharm Res Pract 4: 79-89.
- Carbone S, Canada JM, Billingsley HE, Siddiqui MS, Elagizi A, et al. (2019) Obesity paradox in cardiovascular disease: where do we stand? Vasc Health Risk Manag 15: 89-100.
- Koliaki C, Liatis S, Kokkinos A (2019) Obesity and cardiovascular disease: revisiting an old relationship. Metabolism 92: 98-107.
- De Lorenzo A, Gratteri S, Gualtieri P, Cammarano A, Bertucci P, et al. (2019) Why primary obesity is a disease? J Transl Med 17(1): 169.
- Nuffer, Monika (2019) “Integrative Health and Medicine: Dietary Supplements and Modalities for the Treatment of Obesity.” Nutrition in the Prevention and Treatment of Abdominal Obesity pp. 393-408.
- Butryn ML, Webb V, Wadden TA (2011) Behavioral treatment of obesity. Psychiatr Clin North Am 34(4): 841- 859.
- Sanyal D, Raychaudhuri M (2016) Hypothyroidism and obesity: An intriguing link. Indian J Endocrinol Metab 20(4): 554-557.
- Fruh SM (2017) Obesity: Risk factors, complications, and strategies for sustainable long-term weight management. J Am Assoc Nurse Pract 29(1): 3-14.
- Tsai, Adam Gilden, and Daniel H. Bessesen (2019) “Obesity.” Annals of Internal Medicine 170(5).
- Tsai AG (2019) Why I Treat Obesity. Perm J 23.
- Garber, Abrahamson MJ, Barzilay JI, Blonde L, Bloomgarden ZT, et al. (2013) “AACE Comprehensive Diabetes Management Algorithm 2013.” Endocrine Practice 19(2): 327-336.
- DeGeeter Michelle, Ece Ilkiz Okarlton, Jamie Ellex, Christian Dolder. (2018) “Results of a Pharmacist Intervention on Weight Parameters and A1c Compared to Standard Patient Care.” J Pharm Technol 34(5): 194-198.
- Zanni GR (2014) Hyperlipidemia: Updated Guidelines Impact Counseling. Pharmacy Times.
- Hetro A, Rossetto J, Bahlawan N, Ryan M (2003) Clinical pharmacists supporting patients with diabetes and/or hyperlipidemia in a military medical home. J Am Pharm Assoc 55(1): 73-76.
- Tsuyuki RT, Rosenthal M, Pearson GJ (2016) A randomized trial of a community-based approach to dyslipidemia management: Pharmacist prescribing to achieve cholesterol targets (RxACT Study). Can Pharm J (Ott) 149(5): 283-292.
- Oriordan M (2016) Pharmacist Management of High Cholesterol Gets More Patients to Goal, Lowers LDL Levels: RxACT. TCTMD News.
- Joel C Mars (2010) Pharmacy Perspectives in Dyslipidemia Management. US Pharmacisty.
- Cassagnol Manouchkathe, Ezzo D, Patel PN (2013) New Therapeutic Alternatives for the Management of Dyslipidemia. Journal of Pharmacy Practice 26(6): 528-540.
- Lewis A, Torvinen S, Dekhuijzen PN, Chrystyn H, Watson AT, et al. (2016) The economic burden of asthma and chronic obstructive pulmonary disease and the impact of poor inhalation technique with commonly prescribed dry powder inhalers in three European countries. BMC Health Serv Res 16: 251.
- Xin C, Xia Z, Jiang C, Lin M, Li G (2016) The impact of pharmacist-managed clinic on medication adherence and health-related quality of life in patients with COPD: a randomized controlled study. Patient Prefer Adherence 10: 1197-1203.
- Usmani OS (2019) Choosing the right inhaler for your asthma or COPD patient. Ther Clin Risk Manag 15: 461-472.
- Mubarak N, Hatah E, Khan TM, Zin CS (2019) A systematic review and meta-analysis of the impact of collaborative practice between community pharmacist and general practitioner on asthma management. J Asthma Allergy 12: 109-153.
- Duong TN, Zeki AA, Louie S (2017) Medical Management of Hospitalized Patients with Asthma or Chronic Obstructive Pulmonary Disease. Hosp Med Clin 6(4): 437-455.
- Krishnan JA, Nibber A, Chisholm A, Price D, Bateman ED, et al. (2019) Prevalence and Characteristics of Asthma-Chronic Obstructive Pulmonary Disease Overlap in Routine Primary Care Practices. Ann Am Thorac Soc 16(9): 1143-1150.
- López-Campos JL, Quintana Gallego E, Carrasco Hernández L (2019) Status of and strategies for improving adherence to COPD treatment. Int J Chron Obstruct Pulmon Dis 14: 1503-1515.
- Jardim JR, Nascimento OA (2019) The Importance of Inhaler Adherence to Prevent COPD Exacerbations. Med Sci (Basel) 7(4): 54.
- Abdulsalim S, Unnikrishnan MK, Manu MK, Alsahali S, Alrasheedy AA, et al. (2019) Impact of a Clinical Pharmacist Intervention on Medicine Costs in Patients with Chronic Obstructive Pulmonary Disease in India. Pharmacoecon Open.
- McGurran MA, Richter LM, Leedahl ND, Leedahl DD (2019) Impact of a Comprehensive COPD Therapeutic Interchange Program on 30-Day Readmission Rates in Hospitalized Patients. P T 44(4): 185-191.
- Cawley MJ, Warning WJ (2018) Impact of a Pharmacist-driven Spirometry Clinic Service within a Community Family Health Center: A 5-year Retrospective Review. J Res Pharm Pract 7(2): 88-94.
- Ottenbros S, Teichert M, de Groot R, Griens F, Sodihardjo F, et al. (2014) Pharmacist-led intervention study to improve drug therapy in asthma and COPD patients. Int J Clin Pharm 36(2): 336-344.
- Usmani OS, Lavorini F, Marshall J, Dunlop WCN, Heron L, et al. (2018) Critical inhaler errors in asthma and COPD: a systematic review of impact on health outcomes. Respir Res 19(1): 10.
- Kuipers E, Wensing M, Wong-Go E, Daemen BJG, De Smet PAGM, et al. (2019) Adherence to guideline recommendations for asthma care in community pharmacies: actual and needed performance. NPJ Prim Care Respir Med 29(1): 26.
- Deeks LS, Kosari S, Boom K, Peterson GM, Maina A, et al. (2018) The Role of Pharmacists in General Practice in Asthma Management: A Pilot Study. Pharmacy (Basel) 6(4): 114.
- Hunt V, Anderson D, Lowrie R, Montgomery Sardar C, Ballantyne S, et al. (2018) A non-randomised controlled pilot study of clinical pharmacist collaborative intervention for community dwelling patients with COPD. NPJ Prim Care Respir Med 28(1): 38.
- Twigg MJ, Wright DJ (2017) Community pharmacy COPD services: what do researchers and policy makers need to know? Integr Pharm Res Pract 6: 53-59.
- Greenhalgh T, Macfarlane F, Steed L, Walton R (2016) What works for whom in pharmacist-led smoking cessation support: realist review. BMC Med 14(1): 209.
- Kadam NS, Chiplonkar SA, Khadilkar AV, Khadilkar VV (2018) Prevalence of Osteoporosis in Apparently Healthy Adults above 40 Years of Age in Pune City, India. Indian J Endocrinol Metab 22(1): 67-73.
- Patel D, Worley JR, Volgas DA, Crist BD (2018) The Effectiveness of Osteoporosis Screening and Treatment in the Midwest. Geriatr Orthop Surg Rehabil 9: 2151459318765844.
- Tu KN, Lie JD, Wan CKV, Cameron M, Austel AG, et al. (2018) Osteoporosis: A Review of Treatment Options. 43(2): 92-104.
- Elias MN, Burden AM, Cadarette SM (2011) The impact of pharmacist interventions on osteoporosis management: a systematic review. Osteoporos Int 22(10): 2587-2596.
- Jaleel A, Saag KG, Danila MI (2018) Improving drug adherence in osteoporosis: an update on more recent studies. Ther Adv Musculoskeletal Dis 10(7): 141-149.
- Balkhi B, Seoane-Vazquez E, Rodriguez-Monguio R (2018) Changes in the utilization of osteoporosis drugs after the 2010 FDA bisphosphonate drug safety communication. Saudi Pharm J 26(2): 238-243.
- Lau E, Papaioannou A, Dolovich L, Adachi J, Sawka AM, et al. (2008) Patients' adherence to osteoporosis therapy: exploring the perceptions of postmenopausal women. Can Fam Physician 54(3): 394-402.
- McGreevy JL, Kane MP, Busch RS, Bakst G, ElDeiry S (2003) A pharmacist-run anabolic osteoporosis clinic: An abaloparatide descriptive report. J Am Pharm Assoc 59(4): 593-597.
- Cho H, Byun JH, Song I, Kim HY, Ha YC, et al. (2018) Effect of improved medication adherence on health care costs in osteoporosis patients. Medicine (Baltimore) 97(30): 11470.
- Ivanova S, Vasileva L (2017) Current and Emerging Strategies in Osteoporosis Management. Curr Pharm Des 23(41): 6279-6287.
- Leslie WD, Morin SN, Martineau P, Bryanton M, Lix LM (2019) Association of Bone Density Monitoring in Routine Clinical Practice with Anti-Osteoporosis Medication Use and Incident Fractures: A Matched Cohort Study. J Bone Miner Res.
- Tit DM, Bungau S, Iovan C, Nistor Cseppento DC, Endres L, et al. (2018) Effects of the Hormone Replacement Therapy and of Soy Isoflavones on Bone Resorption in Postmenopause. J Clin Med 7(10): 297.
- Fait T (2019) Menopause hormone therapy: latest developments and clinical practice. Drugs Context 2(8): pp. 212551.
- Zuo H, Sun A, Gao L, Xue W, Deng Y, et al. (2019) Effect of Menopausal Hormone Therapy on Bone Mineral Density in Chinese Women: A 2-Year, Prospective, Open-Label, Randomized-Controlled Trial. Med Sci Monit 25: 819-826.
- Bowers BL, Drew AM, Verry C (2018) Impact of Pharmacist-Physician Collaboration on Osteoporosis Treatment Rates. Ann Pharmacother 52(9): 876-883.
- Duquet N (2014) [Osteoporosis: treatment and pharmaceutical care]. J Pharm Belg (2): 14-24.
- Uhlig HH (2013) Monogenic diseases associated with intestinal inflammation: implications for the understanding of inflammatory bowel disease. Gut 62(12): 1795-1805.
- Cury DB, Oliveira R, Cury MS (2019) Inflammatory bowel diseases: time of diagnosis, environmental factors, clinical course, and management - a follow-up study in a private inflammatory bowel disease center (2003-2017). J Inflamm Res 12: 127-135.
- Bon L, Scharl S, Vavricka S, Rogler G, Fournier N, et al. (2019) Association of IBD specific treatment and prevalence of pain in the Swiss IBD cohort study. PLoS One 14(4): 0215738.
- Aniwan S, Harmsen WS, Tremaine WJ, Loftus EV Jr (2019) Incidence of inflammatory bowel disease by race and ethnicity in a population-based inception cohort from 1970 through 2010. Therap Adv Gastroenterol 12: 1756284819827692.
- Ye BD, Travis S (2019) Improving the quality of care for inflammatory bowel disease. Intest Res 17(1): 45-53.
- Lichtenstein GR, Shahabi A, Seabury SA, Lakdawalla DN, Espinosa OD, et al. (2019) Lifetime Economic Burden of Crohn's Disease and Ulcerative Colitis by Age at Diagnosis. Clin Gastroenterol Hepatol 1542-3565(19)30765-7.
- Barrett K, Glatter J (2019) New standards for IBD aim to improve patient experience and outcomes. Guidelines in Practice (Gastrointestinal) UK.
- Sood A, Ahuja V, Kedia S, Midha V, Mahajan R, et al. (2019) Diet and inflammatory bowel disease: The Asian Working Group guidelines. Indian J Gastroenterol 38(3): 220-246.
- Rizzello F, Spisni E, Giovanardi E, Imbesi V, Salice M, et al. (2019) Implications of the Westernized Diet in the Onset and Progression of IBD. Nutrients 11(5): 1033.
- Malekzadeh MM, Sima A, Alatab S, Sadeghi A, Daryani NE, et al. Iranian Registry of Crohn's and Colitis: study profile of first nation-wide inflammatory bowel disease registry in Middle East. Intest Res 17(3): 330-339.
- Choi K, Chun J, Han K, Park S, Soh H, et al. (2019) Risk of Anxiety and Depression in Patients with Inflammatory Bowel Disease: A Nationwide, Population-Based Study. J Clin Med 8(5): pp. 654.
- Panhwar MS, Mansoor E, Al-Kindi SG, Sinh P, Katz J, et al. (2019) Risk of Myocardial Infarction in Inflammatory Bowel Disease: A Population-based National Study. Inflamm Bowel Dis 25(6): 1080-1087.
- Kuenzig ME, Bishay K, Leigh R, Kaplan GG, Benchimol EIet al. (2018) Co-occurrence of Asthma and the Inflammatory Bowel Diseases: A Systematic Review and Meta-analysis. Clin Transl Gastroenterol 9(9): 188.
- Vutcovici M, Brassard P, Bitton A (2016) Inflammatory bowel disease and airway diseases. World J Gastroenterol 22(34): 7735-7741.
- Kelly OB, Li N, Smith M, Chan J, Inman RD, et al. (2019) The Prevalence and Clinical Associations of Subclinical Sacroiliitis in Inflammatory Bowel Disease. Inflamm Bowel Dis 25(6): 1066-1071.
- Scharl S, Barthel C, Rossel JB, Biedermann L, Misselwitz B, et al. (2019) Malignancies in Inflammatory Bowel Disease: Frequency, Incidence and Risk Factors-Results from the Swiss IBD Cohort Study. Am J Gastroenterol 114(1): 116-126.
- Waters BM, Jensen L, Fedorak RN (2005) Effects of formal education for patients with inflammatory bowel disease: a randomized controlled trial. Can J Gastroenterol 19(4): 235-44.
- Ashok K, Mathew AA, Thomas A, Mohan D, Gopalakrishna R, et al. (2017) Clinical Pharmacist’s Interventions on Medication Adherence and Knowledge of Inflammatory Bowel Disease Patients. J Young Pharm 9(3): 381-385.
- Tiao DK, Chan W, Jeganathan J, Chan JT, Perry J, et al. (2017) Inflammatory Bowel Disease Pharmacist Adherence Counseling Improves Medication Adherence in Crohn's Disease and Ulcerative Colitis. Inflamm Bowel Dis 23(8): 1257-1261.
- McDowell C, Haseeb M (2019) Inflammatory Bowel Disease (IBD) In: Stat Pearls [Internet].
- Jones ASC (2014) Optimizing therapy for inflammatory bowel disease. Clinical Pharmacist.
- Steel A, Morgan H, Tan W, Vanessa Marvin, Mahmood Wahed (2018) PTU-140 Does a dedicated inflammatory bowel disease (IBD) pharmacist clinic improve patient safety? 67: 265-266.
- Bhat S (2015) The Pharmacist's Role in Biologic Management for IBD in a Health System-Integrated Practice Model. Pharmacy Times.



 We use cookies to ensure you get the best experience on our website.
We use cookies to ensure you get the best experience on our website.